Scroll to:
Application of alginate polymer polysaccharide hemostatic hydrogel for ongoing arterial bleeding from peptic ulcer of gastroenteroanastomosis (A clinical case)
https://doi.org/10.47183/mes.2025-243
Abstract
Introduction. Treatment of ulcer gastroduodenal bleeding is a challenging problem of emergency surgery. The combined technique of endoscopic hemostasis in ongoing arterial ulcer bleeding reduces the rate of recurrences in only 21.3% of cases, which indicates the need for improved endoscopic hemostasis technologies. In this regard, the use of triple therapy based on conventional methods (injections, coagulation, clipping) and local hemostatic systems seems promising.
Clinical case description. We describe a clinical case of ongoing arterial ulcer bleeding from a peptic ulcer of gastroenteroanastomosis treated by endoscopic hemostasis using a 5% solution of aminocaproic acid with adrenaline in combination with argon plasma coagulation and pneumatic insufflation of an alginate polymer polysaccharide hemostatic hydrogel on the bleeding site.
Conclusions. The use of a personalized approach to endoscopic hemostasis of arterial bleeding from peptic ulcer of gastroenteroanastomosis using an alginate polymer polysaccharide hemostatic hydrogel as part of combined therapy improves the treatment outcome by ensuring final hemostasis, avoiding emergency surgery for massive bleeding, and facilitating the healing process of the ulcerous defect.
Keywords
For citations:
Barannikov S.V., Cherednikov E.F., Polubkova G.V., Banin I.N., Bolkhovitinov A.E., Berezhnoy S.I., Slyusareva E.E. Application of alginate polymer polysaccharide hemostatic hydrogel for ongoing arterial bleeding from peptic ulcer of gastroenteroanastomosis (A clinical case). Extreme Medicine. 2025;27(2):235-242. https://doi.org/10.47183/mes.2025-243
INTRODUCTION
Peptic ulcer disease (PUD) of the stomach and duodenum is a widespread problem affecting mainly young and able-bodied patients. From 2006 to 2017, the occurrence and prevalence of PUD in the Russian Federation decreased from 128.7 to 79.5 per 100,000 population1. However, its complication rate shows no downward trend. The most common PUD complication is gastrointestinal bleeding. According to Amiran S. Revishvili, the Chief Surgeon of the Russian Federation, 47,224 cases of ulcer upper gastrointestinal bleeding (UGIB) were registered in 2023 in Russia, with the total mortality rate of 1.49–17.81%. The postoperative mortality rate reached the level of 6.17–62.5%2.
Patients with bleeding peptic ulcers of gastroenteroanastomosis (GEA) form a separate group. According to statistical data, the current incidence of post-gastrectomy peptic ulcers ranges within 0.5–15%. At the same time, about 90–98% of GEA peptic ulcers are known to develop after partial gastrectomy for duodenal ulcers (DU). The main reasons for the formation of GEA peptic ulcers include preservation gastrectomy (less than 2/3 of the stomach); reservation of a part of the antrum gastric mucosa in the duodenal stump after Billroth II operation; vagus hypertonus and incomplete vagotomy if performed in combination with preservation gastrectomy; adverse effects of the biliary and pancreatic secretions on the gastric stump mucosa in anastomoses other than isolated Roux loop. Complications of GEA peptic ulcers are observed in 75–80% of patients, presenting a significant healthcare problem. Gastrointestinal bleeding is one of the most common complications of GEA peptic ulcers [1][2].
UGIB patients with ongoing arterial bleeding are classified as Forrest Ia cases according to J. Forrest’s Classification for Bleeding Peptic Ulcer [3]. In the structure of UGIB, this type of bleeding accounts for about 7.7% of cases; however, their treatment is associated with significant difficulties. In the management of such patients, it is extremely important to reliably stop the ongoing arterial UGIB and create conditions for the prevention of its recurrence [4][5].
Despite the recent progress in the development of endovascular hemostasis technologies, therapeutic endoscopy remains to be the leading approach to the treatment of such patients. The modern methods of endoscopic hemostasis (EH) for ongoing arterial ulcer UGIB include injectable, physical, mechanical, and combined EH. Endoscopic injections around the bleeding site with various solutions reduce or eliminate arterial ulcer UGIB due to vasoconstriction and local tamponade. The effectiveness of injectable EH in ongoing bleeding reaches 85–92%. However, injectable monotherapy is not recommended due to its temporary effect and a high rate of recurrences that reach about 17.6–24.0%. Argon plasma coagulation (APC) occupies a special place among the EH physical methods. This non-contact method does not involve welding of the diathermy probe (electrode) to the coagulation scab. The effectiveness of APC in primary EH reaches 95–100%. At the same time, the APC method possesses a number of drawbacks: thus, similarly to other coagulation techniques, the violation of the protocol may lead to perforation of the organ wall and bleeding relapses, which are observed in 12.5–25.0% of cases [6][7].
Clipping, i.e., constriction of the bleeding point by a metal clip, is an effective EH approach in the case of arterial ulcer UGIB. The EH using clips is similar to the surgical retroclusion of a bleeding vessel. The clip is passed through the instrumental channel of the endoscope and fixed by a clip applier across the vessel, thereby reliably stopping the bleeding. Clipping is effective in bleeding from destructed large vessels (more than 2 mm in diameter), as well as in patients with severe hypocoagulation. However, the disadvantage of clipping includes the complexity of its implementation. In addition, endoclips are difficult to use in hard-to-reach anatomical areas, such as the lesser curvature of the stomach, the cardia, and the duodenum posterior wall. The use of endoclips is associated with ulcer UGIB relapses, observed in 8–37% of cases [8][9].
Combined EH is currently considered to be the most advanced EH of arterial ulcer UGIB. Injections around the bleeding site with subsequent clipping of the destructed vessel or injections in combination with APC are often used. Combination (dual) therapy, i.e., infiltration in combination with coagulation of the bleeding point or mechanical compression using hemoclips, remains the endoscopic therapy of choice recommended in the main international clinical guidelines for the treatment of patients with ulcer UGIB. However, according to N.V. Lebedeva, the use of combined EH technologies for ongoing arterial ulcer UGIB is also associated with a high recurrent bleeding rate of about 21.3%, which indicates the need to improve EH technologies [9–11].
The use of hemostatic powders and gels is a promising EH of ulcer UGIB. Hemostatic powders absorb blood, exhibit a mechanical tamponing effect, and activate the blood coagulation cascade [12]. Hemospray (TC-325) and EndoClot endoscopic powder systems have become widespread in clinical practice. However, the action of Hemospray and EndoClot is limited to less than 24 h; moreover, they do not promote tissue regeneration [13]. It should be noted that the Voronezh City Specialized Center for the Treatment of Patients with Gastroduodenal Bleeding (Russia) has accumulated extensive experience in the use of powdered granular sorbents (Sephadex®, Gelevinum, Aseptisorb®, etc.) in the GIB treatment. The application of these sorbents to the bleeding point forms a soft elastic gel, which remains on the surface of the defect for up to four days and improves the healing of gastroduodenal ulcers. However, the use of powdered hemostatic systems in the EH of ongoing arterial ulcer UGIB was shown to have low efficiency [14].
The possibility of applying the Diovine granular sorbent with the Gelplastan and NovoSeven® lyophilizate hemostatic agents in the combined endoscopic treatment of ulcer UGIB was described by M.N. Romantsov et al. This technology produced positive results by reducing the ulcer UGIB recurrence risk to 5.01% and mortality to 1.7% [15].
Japanese scientists T. Uroka, N. Ueda, et al. reported the successful application of innovative EH technology using a gel-like hemostatic matrix for GIB after endoscopic submucous dissection. The gel-like hemostatic matrix is a viscous transparent peptide that forms a sealing layer after contact with tissue or blood. The use of this matrix reduces the need for coagulation to stop gastroduodenal bleeding [16].
The use of a triple therapy, which combines conventional EH methods (injections, coagulation, and clipping) with local hemostatic systems, seems to be a promising direction. One such domestic technology of combined EH of ulcer UGIB consists in the use of an alginate polymer polysaccharide hemostatic hydrogel (APPHH) [17]. Previously, we reported an experimental study into the possibility of using APPHHs in the treatment of bleeding stomach defects [18] and the first experience of APPHH clinical use in the combined endoscopic treatment of unstably stopped ulcer bleeding [19]. The clinical research into the use of APPHHs in a combined EH of ulcer UGIB is currently underway.
In this article, we describe the use of an APPHH in the combined treatment of ongoing arterial ulcer UGIB in a patient with GEA peptic ulcer.
CLINICAL CASE DESCRIPTION
On 13.10.2024 at 7:56 a.m., a 73-year-old patient was urgently admitted the Voronezh City Clinical Emergency Hospital No. 1. On admission, the patient complained of vomiting blood with clots, black tarry stools, discernible weakness, and dizziness.
The patient had been ill since 1995, after a Billroth II partial gastrectomy due to duodenal ulcer profuse bleeding. During the 1995–2023 period, the patient had no gastrointestinal complaints. In 2023, GEA peptic ulcer bleeding was detected, which was surgically treated in Kazan. His state worsened on 13.10.2024 with the following symptoms: discernible weakness, dizziness, fainting, decrease in blood pressure to 90/60 mm Hg, black liquid stools, and vomiting blood with clots. He had a history of acute myocardial infarction, type 2 diabetes mellitus, gout. At the moment of admission, the patient was taking Aspirin® on a regular basis.
Objective data. Examination in the emergency department. On admission, the patient’s condition was severe. Consciousness was clear, 15 points on the Glasgow Coma Scale (GCG), blood pressure (BP) — 90/60 mm Hg, heart rate (HR) — 110 per minute, respiratory rate (RR) — 18 per minute, SPO2 — 98%. The overall health status was severe; the skin was pale. During auscultation of the lungs, vesicular respiration occurred in all pulmonary fields, no wheezing. The heart tones were muted and rhythmic. The tongue was dry, covered with a white coating. The stomach was not swollen. An old postoperative scar on the anterior abdominal wall after an upper-midline incision was present. On palpation, the abdomen was soft and painless in all parts. Infiltrates in the abdominal cavity; liver, spleen, kidneys were not palpated. Peritoneal symptoms were negative in all parts of the abdomen. During percussion, hepatic dullness was normal, displaced dullness of percussion sound in the lateral abdominal regions was not detected. Normal peristaltic sounds were listened by auscultation. No costovertebral angle tenderness. Per rectum: traces of liquid black feces on the glove. A nasogastral tube was inserted, and altered blood was obtained through the tube. Simultaneously with the emergency care, diagnostic tests were performed in the emergency department: general and biochemical blood tests, hemostasis system examination, blood type and Rh factor determination, electrocardiographic examination, abdominal ultrasonography and examination by a therapist.
Predominant diagnosis: peptic ulcer of gastroenteroanastomosis with bleeding (ICD 10 — K28.4, chronic or unspecified gastrojejunal ulcer with hemorrhage). Complication of the main diagnosis: severe haemorrhage (A.I. Gorbashko, 1982), 3 Grade blood loss anemia.
Secondary diagnosis: coronary heart disease; postinfarction and atherosclerotic cardiosclerosis; coronary artery aortic atherosclerosis; stage 3 hypertension; Class I chronic heart failure, functional class I; diabetes mellitus type 2; individual target HbA1c level less than 7.5%; myocardial dystrophy; diabetic polyneuropathy; diabetic encephalopathy; gout is not acute.
Medical interventions. Emergency esophagogastroduodenoscopy (EGDS) was performed urgently (30 minutes after admission) (Fig. 1).
Examination of gastroenteroanastomosis (Billroth II operation): the gastric remnant contained a moderate amount of altered blood, which made a detailed examination difficult. The gastric folds were low, longitudinal-and-convoluted, and expanded by air. Peristalsis was satisfactory, with smooth waves in all parts. The mucosa closer to the gastroenteroanastomosis was covered with fresh blood. Gastroenteroanastomosis was wide and freely passable; incomplete visualization of the mucous membrane due to blood residues was noted. In the anastomotic spur area, a spurting bleeding from a destructed vessel 1.0 mm in diameter was noted, the base of the vessel was not brought into the field of view (Fig. 1A). A 5% solution of aminocaproic acid with 0.1% epinephrine solution was injected paravasally into the area of the anastomosis using a disposable endoscopic injector with a needle diameter of 0.7 mm and a needle length of 4 mm until an infiltrate was created (Fig. 1B). The massive bleeding was stopped. After washing, a flat-surface ulcerous defect 7 mm in diameter and 1.5 mm deep was revealed on the anastomosis spur, with a fixed blood clot 5 mm in diameter at the bottom. An attempt to remove the clot with an irrigator and visualize the destructed vessel had no effect. Clipping was technically impossible.
The APC of the bleeding point through the clot was performed using an electrosurgical coagulator with ERBE APC 2 (Elektromedizin) accessories: operating mode FORCED APC, power 30 W (max), flow rate 1.0 L/min; probe for argon plasma coagulation — Flexible Argonsonde REF 932-149 (BOWA), diameter 2.3 mm. Diffuse blood leakage was noted after APC (Fig. 1B). In order to achieve final hemostasis to the bleeding point using an endoscopic pump for pumping an air mixture (EndoClot Air Compressor, EPAC-2, EndoClot Plus. Inc., USA), in an air supply mode of 1.3 L/min through an endoscopic catheter 2.5 mm of diameter, insufflation of powdered APPHH was performed in the amount of 0.5 g. After insufflation to the bleeding point, upon contact with blood and mucus, the powdered hemostatic was actively soaked in blood, turning into a hydrogel. The final hemostasis had been achieved; blood leakage had been stopped (Fig. 1 D).
Further treatment was carried out in the intensive care unit (ICU). The patient refused to perform endoscopic monitoring after the EH. A nasogastric tube was used to control the recurrence of GIB.
On the day 3 of inpatient treatment (15.10.2024), a control EGDS was performed (Fig. 2). The gastric remnant contained a moderate amount of foamed bile. No blood and hematin was present. The ulcerous defect on the anastomosis spur was 0.7 cm in diameter, superficial, and the ulcer base was covered with an alginate hydrogel soaked in bile (Fig. 2A). The hydrogel was removed, and fibrin was present at the ulcer base. In order to prevent recurrence of bleeding and cytoprotective treatment for the ulcerous defect using an endoscopic pump to inject an air mixture in an air supply mode of 1.3 L/min through an endoscopic catheter 2.5 mm of diameter, APPHH insufflation in the amount of 0.5 g was performed (Fig. 2B). A rapid test for the presence of Helicobacter pylori was positive. After the dynamic EGDS, the patient was transferred to a general ward.
During the following three days, the patient’s status remained unchanged. On day 6 of inpatient treatment (18.10.2024), a control EGDS was performed (Fig. 3).
No traces of blood or hematin in the examined sections of the gastric remnant (foamed bile) were noted. The ulcer of the gastroenteroanastomosis spur decreased in size to 5×4 mm, superficial, covered with a transparent hydrogel soaked in bile (Fig. 3A), after which the hydrogel was removed (Fig. 3B). The ulcer base was covered with fibrin with islands of granulation tissue; marginal epithelialization was observed.
In order to prevent bleeding and cytoprotective treatment using an endoscopic pump for pumping an air mixture in an air supply mode of 1.3 L/min through an endoscopic catheter 2.5 mm of diameter, APPHH insufflation was performed (Fig. 3C, D). The patient was discharged from the hospital and forwarded for outpatient treatment to a polyclinic at his place of residence. On 29.10.2024, a control EGDS was performed at the outpatient stage of treatment (Fig. 4).
On examination: the stomach was resected according to the Billroth II type, its stump was small, the gastroenteroanastomosis did not gape widely. A delicate whitish linear scar on the gastroenteroanastomosis spur was seen. The patient had a moderate risk of recurrent gastroduodenal bleeding according to the digital program “Prevention of gastroduodenal bleeding: an individualized risk assessment scheme, the formation of recommendations on patient management tactics” [20]. The patient was given personalized recommendations for the prevention of recurrent gastroduodenal bleeding.
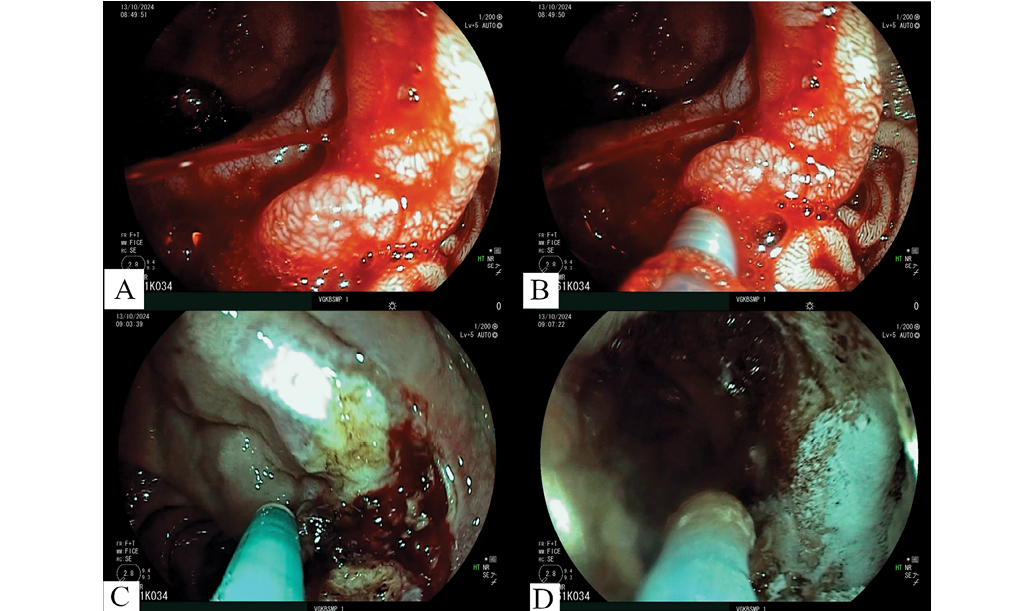
Photo taken by the authors
Fig. 1. Endoscopic images of gastroenteroanastomosis, white light examination: A — ulcerous defect of gastroenteroanastomosis with massive spurting bleeding from the destructed vessel; B — injection compression of the destructed vessel; C — argon plasma coagulation of the bleeding point; D — APPHH insufflation for the ulcerous defect
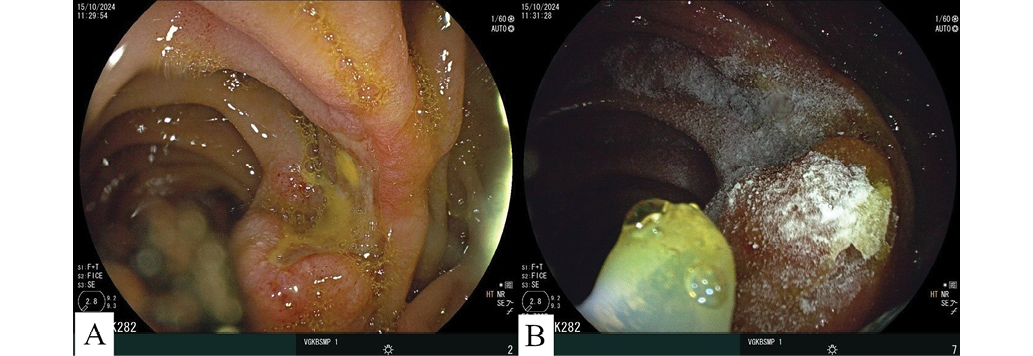
Photo taken by the authors
Fig. 2. Endoscopic images of gastroenteroanastomosis on day 3 of inpatient treatment, white light examination: А — fixed APPHH soaked in bile in the area of the ulcerous defect; B — additional APPHH insufflation for ulcerous defec.

Photo taken by the authors
Fig. 3. Endoscopic images of gastroenteroanastomosis on day 6 of inpatient treatment, white light examination: A — fixed APPHH soaked in bile in the area of the ulcerous defect; B — ulcerous defect on the gastroenteroanastomosis spur after washing the APPHH; C — the onset of APPHH insufflation for ulcerous defect; D — fixed APPHH in the area of the ulcerous defect
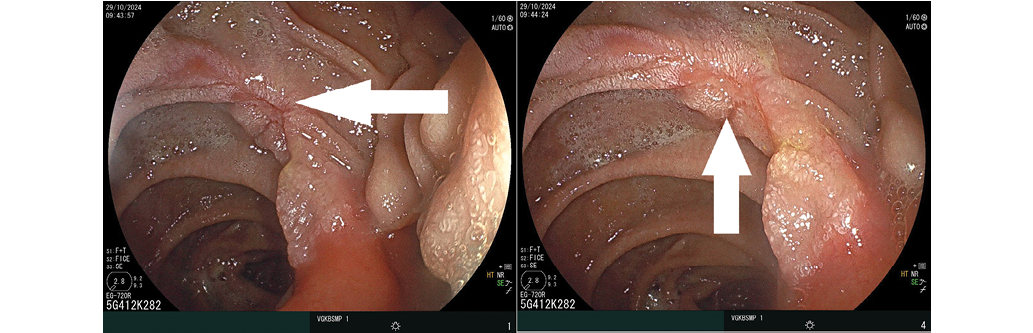
Photo taken by the authors
Fig. 4. Endoscopic images of gastroenteroanastomosis on day 17 of treatment, white light examination. The arrow indicates a delicate whitish linear scar on the gastroenteroanastomosis spur
CLINICAL CASE DISCUSSION
The number of patients with PUD in the Russian Federation is demonstrating a pronounced downward trend, largely due to the current achievements of the state programs. These include a medical examination program with a wide population coverage, the availability of endoscopic examination, as well as the use of highly effective treatment regimens. However, the rate of complicated forms of peptic ulcer disease, and above all, ulcer UGIB, remains at a high level in Russia, showing no reduction in recent years3.
Modern surgical achievements in the treatment of ulcer UGIB (EH, improvement of drug-induced hemostasis, endovascular hemostasis, etc.) have significantly improved the treatment outcomes of patients with ulcer UGIB. However, in situations where ulcer UGIB cannot be stopped using conservative methods, surgeons are forced to perform emergency surgery under the conditions of massive bleeding. The main types of surgical interventions in such patients are retroclusion of a bleeding vessel in an ulcer and, less often, partial gastrectomy [21][22].
At present, there is no doubt that therapeutic endoscopy plays a leading role in the treatment of patients with ulcer UGIB. The international community is actively engaged in the development and application of local hemostatic systems in the form of powders, gels, etc., for the treatment of gastroduodenal ulcer bleeding [23]. Most modern powdered endoscopic systems are non-Russian products. The development of domestic endoscopic hemostasis technologies is an important direction in the context of raising the technological sovereignty and leadership of the country. This highlights the importance of exploring the possibility of using alginate polymer polysaccharide hemostatic hydrogels (APPHHs) in clinical practice.
Alginate polymer polysaccharide hemostatic hydrogel is a powdered, finely dispersed hemostatic agent, the derivatives of which are sodium alginate, potassium sorbate, sodium benzoate, iodoform, and tricalcium phosphate. Upon contact with the bleeding surface and mucus, this hemostatic turns into a hydrogel followed by its tight adhesion to the area of the bleeding point, which provides for prolonged local hemostasis. Preliminary experimental studies into the use of APPHH in the treatment of stomach bleeding have shown its efficacy in stopping experimental bleeding and facilitating the healing process of upper digestive tract defects, which was confirmed by morphological studies [18].
It is important to note that PUD is a chronic disease, which makes the healing quality of the ulcerous defect particularly important in the treatment of gastroduodenal ulcers. According to L.I. Aruin, it is the rough scar that acts as the pathomorphological substrate for PUD exacerbation [24].
In the present article, we describe the experience of using APPHH in the combined treatment of ongoing arterial ulcer UGIB. The discussed clinical case was complicated by massive arterial ulcer UGI, which was treated using a combined EH by injections to the bleeding point followed by APC of the destructed vessel. Following APC, diffuse blood leakage persisted, and the endoscopist had the opportunity to continue APC of the bleeding point. It should be borne in mind that intensive prolonged coagulation can lead to perforation of the hollow organ wall and the development of peritonitis. This complication is extremely serious and can lead to death against the background of acute blood loss. The APPHH application to the bleeding defect allowed us to solve the problem of blood leakage and achieve final hemostasis. Repeated EGDS revealed the absence of bleeding relapses and pronounced cytoprotective properties of APPHH. Due to its pronounced adhesive properties, the APPHH composition used remained on the ulcerous defect for up to three days. EGDS on day 6 revealed signs of ulcerous defect healing in the form of marginal epithelialization, and on day 17, complete healing of the GEA peptic ulcer in the form of a delicate scar.
Summarizing the presented clinical case, the use of a personalized approach to endoscopic hemostasis of arterial bleeding from GEA peptic ulcer in a patient with severe somatic pathology and a high-degree surgical risk, the use of APPHH as part of combined therapy improved the treatment outcome by ensuring final hemostasis, avoiding urgent surgery for massive bleeding, and improving the healing quality of the ulcerous defect. These aspects are extremely important in the treatment of UGIB patients with various concomitant somatic pathologies. In such patients, the impossibility to stop bleeding using conservative methods often requires surgical interventions, which may lead to fatal outcomes.
CONCLUSION
The use of an alginate polymer polysaccharide hemostatic hydrogel (APPHH) as part of the combined endoscopic treatment of ongoing ulcer UGIB ensured reliable hemostasis and allowed recurrent bleeding and emergency surgery to be avoided. It should be noted that this publication describes the first experience of using APPHH technology in a patient with ongoing arterial bleeding from a GEA peptic ulcer. The accumulation of data from larger patient cohorts and their detailed analysis will elucidate the feasibility and effectiveness of this EH technology for clinical surgical practice.
1. Clinical guidelines for Peptic Ulcer disease. Ministry of Health of the Russian Federation; 2024.
2. Revishvili AS, Olovyannyi VE, Gogia BS, Gurmikov BN, Markov PV, Ruchkin DV, et al. Surgical care in the Russian Federation. Мoscow. 2024.
3. Kotova EG, Kobyakova OS, Alexandrova GA, Golubev NA, Oskov YuI, Polikarpov AV, Shelepova EA. Morbidity of the entire Russian population in 2021: statistical materials. Moscow: Central Research Institute of the Ministry of Health of the Russian Federation. 2022.
References
1. Chernousov AF, Horobryh TV, Bogopol’skij P. M. Surgery of peptic ulcer of the stomach and duodenum. Moscow: Prakticheskaya medicina; 2016 (In Russ.).
2. Lyubivyj ED, Kim VL, Lyudovskih IV, Evtihov AV. Treatment of peptic ulcer of gastroenteroanastomosis, complicated by ongoing bleeding. An observation from practice. Bulletin of the Baltic Federal University named after I. Kant. Series: Natural and Medical Sciences. 2021;2:84–92 (In Russ.). EDN: ZEZJTO
3. Forrest JA, Finlayson ND, Shearman DJ. Endoscopy in gastrointestinal bleeding. Lancet. 1974;2(7877):394–7. https://doi.org/10.1016/s0140-6736(74)91770-x
4. Barannikov SV, Cherednikov EF, Yuzefovich IS, Banin IN, Polubkova GV, Vysotskaya AT, et al. Modern Clinical and Epidemiological Features and New Technological Possibilities in the Treatment of Bleeding Gastroduodenal Ulcers. International Journal of Biomedicine. 2021;11(4):428–34. https://doi.org/10.21103/Article11(4)_OA6
5. Vedenin YuI, Mandrikov VV, Oreshkin AYu, Nogina AA, Mikhailichenko GV, Zhulikova SV. Endoscopic hemostasis in gastroduodenal ulcerative bleeding: a regulated approach or personal preferences? Endoscopic Surgery. 2024;30(3):29–33 (In Russ.). https://doi.org/10.17116/endoskop20243003129
6. Lau JYW, Yu Y, Tang RSY, et al. Timing of Endoscopy for Acute Upper Gastrointestinal Bleeding. N Engl J Med. 2020;382(14):1299–308. https://doi.org/10.1056/NEJMoa1912484
7. Lebedev NV, Klimov AE, Barkhudarov AA. Gastroduodenal ulcerative bleeding. Pirogov Russian Journal of Surgery. 2014;8:23–7 (In Russ.).
8. Schmidt A, Gölder S, Goetz M, et al. Over-the-Scope Clips Are More Effective Than Standard Endoscopic Therapy for Patients With Recurrent Bleeding of Peptic Ulcers.Gastroenterology. 2018;155(3):674–86.e6. https://doi.org/10.1053/j.gastro.2018.05.037
9. Lebedev NV, Klimov AE, Moroz VA. Gastroduodenal bleeding. Moscow: Binom; 2015 (In Russ.).
10. Barkun AN, Almadi M, Kuipers EJ, et al. Management of Nonvariceal Upper Gastrointestinal Bleeding: Guideline Recommendations From the International Consensus Group. Ann Intern Med. 2019;171(11):805–22. https://doi.org/10.7326/M19-1795
11. Laine L, McQuaid KR. Endoscopic therapy for bleeding ulcers: an evidence-based approach based on meta-analyses of randomized controlled trials. Clin Gastroenterol Hepatol. 2009;7(1):33–2. https://doi.org/10.1016/j.cgh.2008.08.016
12. Aziz M, Weissman S, Mehta TI, et al. Efficacy of Hemospray in non-variceal upper gastrointestinal bleeding: a systematic review with meta-analysis. Ann Gastroenterol. 2020;33(2):145–54. https://doi.org/10.20524/aog.2020.0448
13. Lee AY, Cho JY. Advancements in hemostatic strategies for managing upper gastrointestinal bleeding: A comprehensive review. World J Gastroenterol. 2024;30(15):2087–90. https://doi.org/10.3748/wjg.v30.i15.2087
14. Cherednikov EF, Barannikov SV, Yuzefovich IS, Chernykh AV, Berezhnova TA, Polubkova GV, et al, Ovsyannikov ES, Shkurina IA. Modern Technologies of Endoscopic Hemostasis in the Treatment of Ulcer Gastroduodenal Bleeding: A Literature Review. International Journal of Biomedicine. 2022;12(1):9–18. https://doi.org/10.21103/Article12(1)_RA1
15. Romantsov MN, Cherednikov EF, Glukhov AA, Fursov KO. New technologies of endoscopic hemostasis in the protocol of treatment of patients with gastroduodenal bleeding. Bulletin of Experimental and Clinical Surgery. 2018;11(1):16–23 (In Russ.). https://doi.org/10.18499/2070-478X-2018-11-1-16-23
16. Uraoka T, Uedo N, Oyama T, et al. Efficacy and Safety of a Novel Hemostatic Peptide Solution During Endoscopic Submucosal Dissection: A Multicenter Randomized Controlled Trial. Am J Gastroenterol. 2023;118(2):276–83. https://doi.org/10.14309/ajg.0000000000002060
17. Barannikov SV, Cherednikov EF, Yuzefovich IS, Banin IN, Bondarenko AA, Maleev YuV. Method of endoscopic hemostasis of a bleeding gastroduodenal ulcer. Patent No. 2762120 C1; 2021 (In Russ.). EDN: DSFKJA
18. Barannikov SV, Cherednikov EF, Shishkina VV, Samoilenko TV, Maleev YuV, Leontiev AV, et al. Morphological characteristics of the healing process in simulated bleeding stomach defects during endoscopic treatment with alginate polymer polysaccharide hemostatic hydrogel. Russian Journal of Evidence-Based Gastroenterology. 2024;13(2):14–24 (In Russ.). https://doi.org/10.17116/dokgastro20241302114
19. Barannikov SV, Cherednikov EF, Polubkova GV, Vorontsov AK, Maleev YuV, Bolkhovitinov AE, et al. First experience of using alginate polymer polysaccharide hemostatic hydrogel in complex endoscopic treatment of unstable gastroduodenal ulcer bleeding: Clinical cases. Kuban Scientific Medical Bulletin. 2024;31(3):73–92 (In Russ.). https://doi.org/10.25207/1608-6228-2024-31-3-73-92
20. Banin IN, Cherednikov EF, Barannikov SV, Yuzefovich IS. Prevention of gastroduodenal bleeding: an individualized risk assessment scheme, the formation of recommendations on patient management tactics Certificate of state registration of the computer program No. 2023667560; 2023 (In Russ.). EDN: BUHKEI
21. Tuerk E, Doss S, Polsley K. Peptic Ulcer Disease. Prim Care. 2023;50(3):351–62. https://doi.org/10.1016/j.pop.2023.03.003
22. Wang A, Yerxa J, Agarwal S, et al. Surgical management of peptic ulcer disease. Curr Probl Surg. 2020;57(2):100728. https://doi.org/10.1016/j.cpsurg.2019.100728
23. Lau LHS, Sung JJY. Treatment of upper gastrointestinal bleeding in 2020: New techniques and outcomes. Dig Endosc. 2021;33(1):83–94. https://doi.org/10.1111/den.13674
24. Aruin LI. The quality of healing of gastroduodenal ulcers: functional morphology, the role of pathogenetic therapy methods. Experimental and clinical gastroenterology. 2006;5:40–50 (In Russ.). EDN: PBZWJR
About the Authors
S. V. BarannikovRussian Federation
Sergey V. Barannikov, Cand. Sci. (Med.)
Voronezh
E. F. Cherednikov
Russian Federation
Evgeniy F. Cherednikov, Dr. Sci. (Med.)
Voronezh
G. V. Polubkova
Russian Federation
Galina V. Polubkova, Cand. Sci. (Med.)
Voronezh
I. N. Banin
Russian Federation
Igor N. Banin, Cand. Sci. (Med.)
Voronezh
A. E. Bolkhovitinov
Russian Federation
Alexey E. Bolkhovitinov
Voronezh
S. I. Berezhnoy
Russian Federation
Sergey I. Berezhnoy
Voronezh
E. E. Slyusareva
Russian Federation
Eva E. Slyusareva
Voronezh
Supplementary files
Review
For citations:
Barannikov S.V., Cherednikov E.F., Polubkova G.V., Banin I.N., Bolkhovitinov A.E., Berezhnoy S.I., Slyusareva E.E. Application of alginate polymer polysaccharide hemostatic hydrogel for ongoing arterial bleeding from peptic ulcer of gastroenteroanastomosis (A clinical case). Extreme Medicine. 2025;27(2):235-242. https://doi.org/10.47183/mes.2025-243

















