Scroll to:
Hyperbaric oxygenation for assisting recovery of athletes including those affected by COVID-19 under medium-altitude conditions
https://doi.org/10.47183/mes.2024-26-3-71-76
Abstract
Introduction. Modern scientific studies demonstrate the effectiveness of hyperbaric oxygenation in assisting recovery following physical exertion including those affected by COVID-19 infection.
Objective. The study sets out to identify the beneficial effects of hyperbaric oxygenation therapy in assisting the recovery of athletes under medium-altitude conditions, including those who have previously undergone COVID-19, by examining respiratory and circulatory systems.
Materials and methods. The study was performed on 39 highly qualified athletes during a period of training in mountainous areas. The athletes’ heart rate variability, central hemodynamics, saturation and external respiration were determined prior to hyperbaric oxygenation, as well as immediately following the procedure, 10 min after the procedure, and following a course of 7 procedures.
Results. According to heart rate variability indices in women who underwent COVID-19, there was a tendency to decrease heart rate 10 min after hyperbaric oxygenation and very a slow wave power index after the course of (before — 665.65 (592.54; 921.07) ms2; after — 541.47 (371.01; 840.89) ms2, p < 0.05). After the first session there was a decrease in systolic blood pressure (before — 117 (111; 120) mm Hg; after — 109 (104; 115) mm Hg, p < 0.03), as well as in the index of volumetric airflow velocity at the moment of exhalation of 50% of forced vital capacity of lungs. A comparison of men’s parameters revealed a decrease in peripheral vascular resistance and blood pressure. In women and men who had previously suffered COVID-19 infection, the index of impaired oxygen uptake from the microcirculation system decreased under the influence of hyperbaric oxygenation.
Conclusions. Hyperbaric oxygenation therapy is a safe and effective method for assisting the recovery of athletes under medium-altitude conditions, including those who have previously suffered COVID-19 infection. The observed improvements in functional state are manifested over the course of application (7 sessions).
Keywords
For citations:
Ter-Akopov G.N., Koryagina Y.V., Abutalimova S.M., Nopin S.V., Kushnareva Y.V. Hyperbaric oxygenation for assisting recovery of athletes including those affected by COVID-19 under medium-altitude conditions. Extreme Medicine. 2024;26(3):71-76. https://doi.org/10.47183/mes.2024-26-3-71-76
INTRODUCTION
Hyperbaric oxygen therapy (HBOT) provides an artificial increase in blood oxygen capacity due to additional dissolution of oxygen in plasma as a result of increase in the partial pressure of oxygen in the inhaled gas mixture related to the total barometric pressure of the external environment [1, 2]. When subjected to HBOT in suboptimal or optimal doses, the human organism switches to a qualitatively new state characterized by economy (hypofunction) of physiological systems [3][4].
Due to the onset of the novel coronavirus COVID-19 pandemic, a need arose for the use of methods to ameliorate complications associated with this disease manifesting as hypoxia and requiring supplemental oxygen support [5]. Thus, the issue of ensuring the safety of HBOT therapy in patients with COVID-19 becomes relevant. The inclusion of daily HBOT sessions (at least 4) in “soft” modes (1.4–1.6 atm.) as part of complex therapy for COVID-19 has demonstrated its safety and a preliminary positive effect on the subjective state of the examined patients and blood oxygen saturation dynamics [6].
According to A.G. Shchurov’s studies, HBOT can be used in various sports to quickly eliminate fatigue resulting from the performed load. This may serve as a preliminary stimulation of performance before training or competitions, as well as for the prevention and elimination of organ and system dysfunctions due to excessive physical overstrain [8]. Published data demonstrate the effectiveness of HBOT for the recovery of patients after COVID-19, as well as for the recovery of athletes after physical exertion. However, no data on the use of HBOT for the recovery of athletes training under hypobaric hypoxia (medium-altitude) conditions, or athletes who have previously suffered COVID-19 infection under such conditions, were found in the available sources.
The study set out to reveal the beneficial effects of hyperbaric oxygenation therapy in the recovery of athletes, including those who had previously contacted COVID-19, under medium-altitude conditions according to the study of respiratory and circulatory systems.
MATERIALS AND METHODS
The study of HBOT effects during training of athletes in the medium-altitude conditions was carried out during training camps at an altitude of 1240 meters in Russia on 39 highly qualified athletes (mean age — 21.5 (18; 25) years; sports qualification — Candidates Masters of Sports and Masters of Sports; mixed groups in sports: sambo, ski racing, figure skating, handball), including 27 women (main group (MG) — 16; control group (CG) –11), and 12 men (7 MG and 5 CG).
As our earlier studies showed, athletes may experience strain of adaptation mechanisms during training in the middle mountains without the use of special means of recovery (HBOT). The observed strain, as manifested in increased sympathetic activity and central hemodynamics, was especially pronounced in athletes who had previously experienced COVID-19 [11][12]. Due to the fact that these data have already been published, the division into MG and CG was based only on the presence of COVID-19 in the anamnesis in the present study. Consequently, athletes with a history of COVID-19 were categorized as MG and those without COVID-19 were categorized as CG. All athletes participating in the study were administered HBOT treatment.
Inclusion criteria: high qualification of athletes, high training loads under medium-altitude conditions. Exclusion criteria: refusal to participate in the study, acute illnesses and injuries, contraindications to HBOT (history of epilepsy, claustrophobia, hyperthermia, uncontrolled arterial hypertension, hypotension, sinusitis, impaired patency of the eustachian tubes and channels connecting the sinuses with the external environment, hypersensitivity to oxygen).
The course of HBOT procedures was carried out in a “BaroOx 1.0” barocamera using a “Covidien LLC” (USA) mask according to a preset program having the following parameters: overpressure — 30 kPa; oxygen content — 93±2 %; air flow rate — 45 L/min; compression/decompression rate — 6 kPa/min; duration of one procedure — 30 min; course — at least 7 procedures (1 procedure per day); body position — half-lying.
The study of central hemodynamics, heart rate variability (HRV) and oxygen parameters (impaired oxygen uptake from the microcirculation system and blood saturation) was performed using the ESTECK System Complex device (LD Technology, USA). The spirometric indices of the athletes were determined using a “Carefusion MicroLab Mk8” spirometer (South Wales, UK).
Statistical processing of the data was performed using the “Statistica 13.0” computer program. A comparison of indicators between the main and control groups was carried out using the Mann-Whitney criterion; indicators of the main and control groups when HBOT was applied to them in dynamics were compared using the nonparametric Wilcoxon criterion. The indicators are presented in the form of medians and quartiles.
RESULTS
When analyzing the data of the HBOT effect, the indicators of athletes before HBOT (baseline), immediately following HBOT administration, 10 min after HBOT, as well as after a course of 7 HBOT sessions, were compared. The baseline MG and CG parameters did not differ statistically significantly. Although the dynamics of heart rate (HR) did not reveal statistically significant changes according to the HRV parameters in women, all women (COVID-19 infected and non-infected) displayed a tendency to decrease HR 10 min after HBOT as compared to the baseline level (Fig. 1A).
The same positive trend was observed for the power index of fast high-frequency (HF) waves, which increased 10 min after administration of HBOT in female athletes who had not previously had COVID-19 (before — 758.38 (585.11; 1015.1) ms2; 10 min after — 1734.57 (998.57; 2086.71) ms2).
The low-frequency (LF) wave power index in female athletes with no previous COVID-19 infection tended to decrease after the HBOT course (before — 731.07 (505.87; 984.3) ms2; immediately after the 1st session — 711.66 (441.24; 894.39) ms2; 10 min after the 1st session — 808.8 (619.2; 1086.15) ms2; after the course — 426.23 (265.4; 940.66) ms2).
The power index of very low frequency waves (VLF) reflecting the work of the slowest level of regulation (suprasegmental or energetic metabolic) in female athletes who had previously undergone COVID-19 decreased by the end of the course (before the course — 665.65 (592.54; 921.07) ms2; after the course — 541.47 (371.01; 840.89) ms2, p < 0.05). In female athletes who had not previously had COVID-19, there was also a tendency for this index to decrease following the HBOT course, but to increase after the 1st session (up to — 665.24 (618.97; 848.75) ms2; immediately after the 1st session — 695.94 (639.81; 992.72) ms2; 10 min after the 1st session — 1219.29 (577.34; 1759.04) ms2; after the course — 620.17 (414; 712.03) ms2). In women who had not previously been infected with COVID-19, there is an additional tendency towards decreased stress index (SI) immediately after the 1st HBOT session (before — 100.3 (73.8; 128.2) conventional units; immediately after the 1st session — 81.55 (39.7; 111.5) conventional units; 10 min after the 1st session — 48.35 (44.9; 113.35) conventional units; after the course — 107.3 (65.1; 149.4) conventional units).
When analyzing the central hemodynamic parameters in women who had previously had COVID-19, a decrease in systolic blood pressure was revealed after the first session (before — 117 (111; 120) mmHg; immediately after the 1st session — 109 (104; 115) mmHg, p < 0.03; 10 minutes after the 1st session — 114 (107; 117) mmHg, p < 0.05; after the course — 114 (108; 122.5) mmHg) (Fig. 1B). The index of impaired oxygen absorption from the microcirculation system VO2 decreased (before — 320 (310; 320) mL/min/m2; immediately after the 1st session — 130 (130; 180) mL/min/m2, p < 0.001; 10 minutes after the 1st session — 130 (130; 130) mL/min/m2, p < 0.001; after the course — 320 (310; 330) mL/min/m2).
In women without a history of COVID-19, a decrease in the stiffness index, which characterizes blood pressure in large arteries, was observed both after one session and after a course of HBOT procedures (before — 6.22 (5.26; 6.86) m/s; immediately after the 1st session — 6.02 (5.27; 6.29) m/s, p < 0.05; 10 minutes after the 1st session — 6.15 (6.02; 6.62) m/s; after the course — 5.94 (5.24; 6.56) m/s, p < 0.05). After the first session, the same group showed a decrease in the PSS (before — 1207.6 (1132.9; 1243.8) MPa*s/m3; immediately after the 1st session — 1180.3 (975.5; 1243.5) MPa*s/m3, p < 0.05; 10 minutes after the 1st session — 1062.9 (823.15; 1330.2) MPa*s/m3, p < 0.05; after the course — 1156.6 (1074.3; 1342.5) MPa*s/m3 (Fig. 34)) and diastolic blood (arterial) pressure (DBP) (before — 67 (64; 74) mmHg, p < 0.05; immediately after the 1st session — 64 (59.5; 69.5) mmHg, p < 0.05; 10 minutes after the 1st session — 65.5 (61.5; 70) mmHg; after the course — 64 (61; 69)) mmHg.
In terms of external respiratory function in women who had previously undergone COVID-19, no significant changes were observed during HBOT application apart from MEF50 (maximal expiratory flow at 50% of forced vital capacity), which significantly decreased (before — 4.99 (4.42; 5.83) L; immediately after — 4.66 (4.09; 5.62) L, p < 0.01), apparently due to relaxation of respiratory muscles. In women with no previous history of COVID-19, forced vital capacity of lungs (FVC) decreased statistically significantly after the HBOT course (before — 4.25 (4; 4.77) L; after the course — 4.13 (3.85; 4.53) L, p < 0.02).
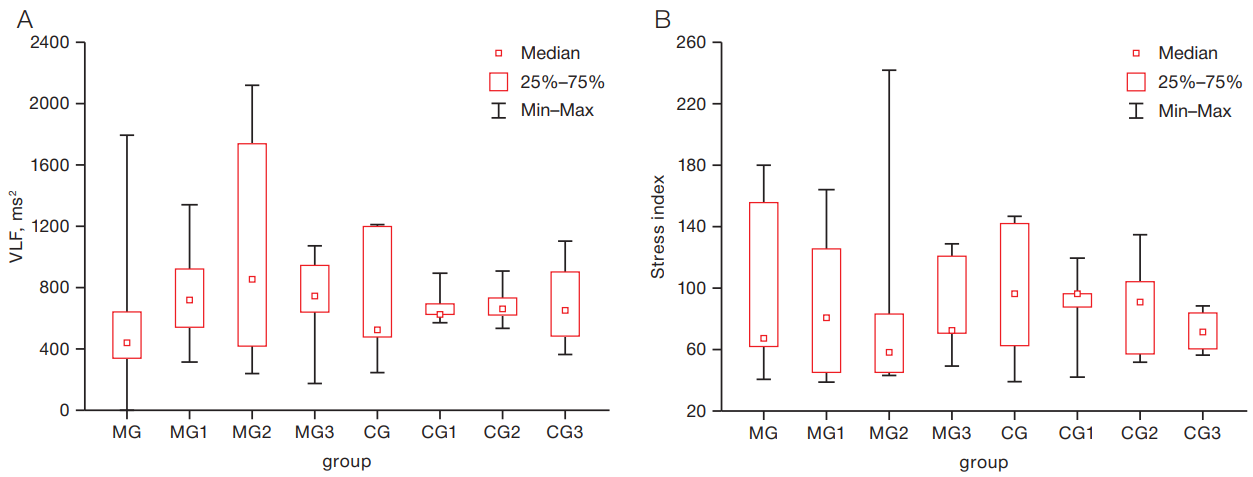
A comparison of HRV indices during HBOT sessions in COVID-19 male athletes with previous COVID-19 revealed a statistically significant increase in the power of very low frequency (VLF) waves (p < 0.05) (Fig. 2A). In male athletes who had not previously had COVID-19, there was a tendency towards decreased stress index after a course of HBOT (up to — 96.2 (61.5; 141.1) conventional units; immediately after the 1st session — 95.6 (86.6; 95.8) conventional units; 10 min after the 1st session — 90.2 (56.3; 103) conventional units; after the course — 70.45 (59.2; 82.8) conventional units (Fig. 2B).
According to the central hemodynamic parameters (Table 1), the peripheral vascular resistance decreased immediately after the first HBOT session (p < 0.05); however, following the course, this parameter returned to the initial values. There was also a tendency towards decreased systolic and diastolic blood pressure. Male athletes who had previously contacted COVID-19 also exhibited statistically significantly decreased impaired oxygen uptake indicator from the VO2 microcirculation system under the influence of HBOT. Both in in men who had previously had COVID-19 and those who did not have a history of COVID-19, spirometry parameters did not change statistically significantly. In male athletes who had not previously had COVID-19, statistically significant differences in heart rate variability (HRV) and central hemodynamic parameters were not revealed during the session or over the course of HBOT.
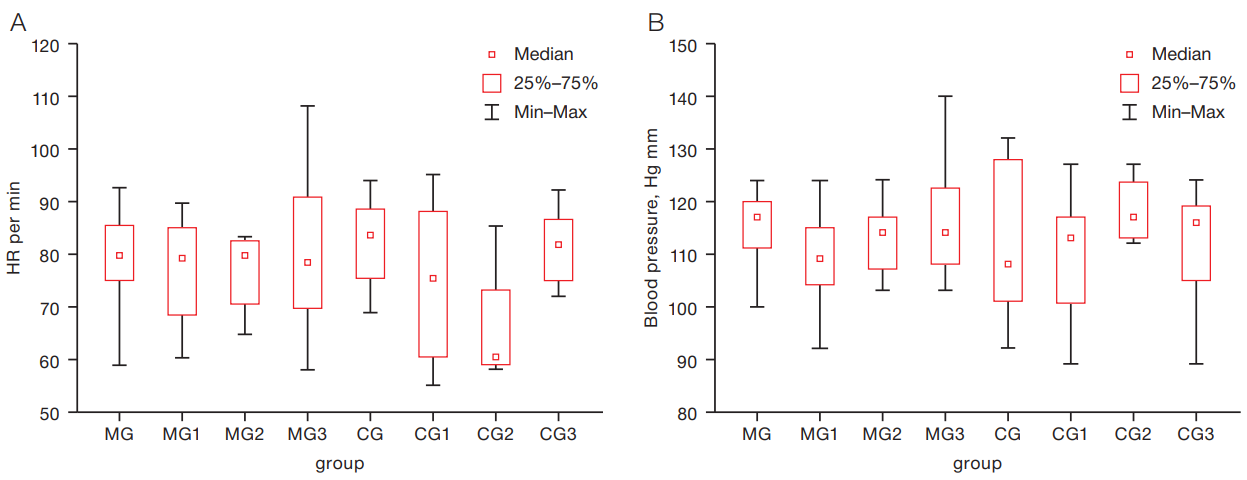
Figure prepared by the authors using their own data
Fig. 1. HRV (A) and Systolic blood pressure (SBP) (B) in highly qualified female athletes with and without COVID-19 under the influence of HBOT: MG — before HBOT sessions; MG1 — immediately after HBOT; MG2 — 10th min after HBOT; MG3 — after HBOT course; CG — before HBOT sessions; CG1 — immediately after HBOT; CG2 — 10th min after HBOT; CG3 — 3 after HBOT course
Figures prepared by the authors using their own data
Fig. 2. VLF (A) and stress index (B) indicators in male athletes with and without COVID-19, under the influence of HBOT: MG — before HBOT, MG1 — immediately after HBOT, MG2 — 10th minute after HBOT, MG3 — after the HBOT course, CG — before HBOT sessions, CG1 — immediately after HBOT, CG2 — 10th minute after HBOT, CG3 — 3 after the HBOT course
Table 1. Indices of central hemodynamics and impaired oxygen uptake from the microcirculation system in male athletes who previously underwent COVID-19 during HBOT application, Me (Q1; Q3), n = 7
|
Indices |
MG |
MG 1 |
MG 2 |
MG 3 |
P |
|
SVR, MPa*s/m3 |
1020.3 (857.9; 1232.5) |
970.3 (822.6; 1247.2) |
972.6 (823.1; 1036.6) |
1045.15 (995.3; 1086.5) |
MG-MG1 < 0.05 |
|
CO, L/min |
7.3 (6.6; 8.4) |
7.5 (6.6; 8.5) |
7.7 (6.8; 8.7) |
7 (6.7; 7.1) |
- |
|
CI, L/min/m2 |
3.4 (3.3; 3.9) |
3.9 (3.2; 3.9) |
3.9 (3.4; 4.2) |
3.55 (3.2; 3.9) |
- |
|
Average blood pressure, mmHg |
92 (90; 95.3) |
87.7 (83; 103) |
90 (83; 103) |
90.65 (87.3; 93) |
- |
|
VO2, mL/min/m2 |
320 (320; 320) |
180 (130; 320) |
190 (130; 320) |
315 (310; 320) |
MG-MG2, MG-MG3 < 0.05 |
|
SBP, mmHg |
127 (120; 136) |
122 (115; 133) |
122 (115; 133) |
123 (120; 129) |
- |
|
DBP, mmHg |
75 (73; 78) |
69 (67; 88) |
73 (67; 88) |
74.5 (71; 78) |
- |
Table prepared by the authors using their own data
Note: VO2 — index of oxygen uptake disturbance from the microcirculation system, SVR — peripheral (systemic) vascular resistance, CO — cardiac output, CI — cardiac index or index of volumetric blood flow velocity, MG — before HBOT, MG1 — immediately after HBOT, MG2 — 10 min after HBOT, MG3 — after HBOT course.
DISCUSSION
Researchers have previously noted not only accelerated recovery of the body as a result of HBOT therapy, but also an expansion of physiological reserves [8]. Significant differences between the groups using HBOT and normobaric oxygenation were observed in blood saturation and tissue saturation indexes [13]. Data in foreign literature describing not always effective use of HBOT for restoring the performance of athletes and recovery from sports injuries [14][15] may be due to the different protocols of the procedures followed.
In our study carried out under medium-altitude conditions, it was found that the use of HBOT does not have an unambiguously positive effect on increasing the functional capabilities of the body, but rather promotes relaxation. Saturation indicators following HBOT did not change (before and after were within normal limits); however, after the 1st session, the indicator of impaired oxygen absorption from the microcirculation system decreases, indicating a beneficial effect and the necessary saturation of tissues with oxygen. The more pronounced positive effects of HBOT in women were particularly evident in the form of increased parasympathetic activity following the entire course. The general condition caused by the increased tone of the parasympathetic division of the autonomic nervous system (ANS) in women manifested itself in a relaxing effect, including on the respiratory muscles.
Currently, the following models of training at different altitudes are known. The classic approach is the “Live high — train high” model, when athletes live and train at the same altitude in mountainous terrain [12][16]. There is also a model of mountain training using hyperoxia, “Live high — train low with additional oxygen”. In this case, athletes train in the mid-altitude zone, but simulate sea level using additional oxygen inhalation [17]. As part of developing the directions of mountain training for athletes based on the obtained data, we propose a new training model designated as “Live high — train high — recover with HBOT”.
CONCLUSION
The use of HBOT in medium-altitude conditions has proven to be a safe and effective method of restoring the body, including in athletes who have previously had COVID-19. However, the use of one session does not have an immediately positive effect in terms of increasing the functionality of the circulatory and respiratory systems; rather, this method is effective when used over the course of at least 7 sessions. Following the first HBOT session, the dynamics of functional indicators in athletes (both those who had been infected with COVID-19 and those who had not) under the influence of HBOT under medium-altitude training conditions was manifested by decreased vascular tone and blood pressure producing a hyperadaptive response. The positive effects of an entire course of HBOT, which were manifested in the form of increased parasympathetic activity, were more pronounced in women, leading to a relaxing effect, including on the respiratory muscles. All athletes experienced improved tissue oxygen saturation. In general, this method is recommended for general recovery of the body following a training day, as well as micro- and mesocycles and during the off-season preparation period. However, the method is not recommended immediately before training sessions and competitions.
References
1. Branco BH, Fukuda DH, Andreato LV, Santos JF, Esteves JV, Franchini E. The Effects of Hyperbaric Oxygen Therapy on PostTraining Recovery in Jiu-Jitsu Athletes. PLoS ONE. 2016;11(3):e0150517. https://doi.org/10.1371/journal.pone.0150517
2. Pustovoit VI, Nikonov RV. Hyperbaric oxygenation in clinical and sports practice. Kremlin Medicine Journal. 2022;1:78–86 (In Russ.). https://doi.org/10.26269/1jtg-0435
3. Baidin SA, Gramenitsky AB, Rubinchik BA. A Guide to Hyperbaric Medicine. Moscow: Medicine; 2008 (In Russ.). EDN: QLRMML
4. Polikarpochkin AN, Levshin IV, Hyperbaric oxygenation in physical rehabilitation after recovery from “COVID-19” infection. Actual problems of physical and special training of law enforcement agencies. 2021;1:225–30 (In Russ.). EDN: VNHKQQ.
5. Levina OA, Еvseev AK, Shabanov AK, Kulabukhov VV, Kutrovskaya NY, Goroncharovskaya IV, et al. The Safety of Hyperbaric Oxygen Therapy in the Treatment of Covid-19. Russian Sklifosovsky Journal “Emergency Medical Care”. 2020;9(3):314–20 (In Russ.). https://doi.org/10.23934/2223-9022-2020-9-3-314-320
6. Chernyak AV, Neklyudova GV, Naumenko ZhK, Pashkova TL. Lung function in athletes involved in skiing and speed skating. Pulmonology. 2019;29(1):62–9 (in Russ.).
7. https://doi.org/10.18093/0869-0189-2019-29-1-62-69
8. Shchurov AG., Dmitriyev GG, Yendaltsev BV. Dinamika vosstanovleniya funktsional′nogo sostoyaniya sportsmenov posle fizicheskoy nagruzki v usloviyakh giperbaricheskoy oksigenatsii. Teoriya i praktika fizicheskoy kultury. 2016;2:37–9 (In Russ.). EDN: VOLNWX
9. Sperlich B, Zinner C, Hauser A, Holmberg HC, Wegrzyk J. The impact of hyperoxia on human performance and recovery. Sports Med. 2017;47(3):429–38. https://doi.org/10.1007/s40279-016-0590-1
10. Ishihara, A. Mild hyperbaric oxygen: mechanisms and effects. J Physiol Sci. 2019;69(4):573–80. https://doi.org/10.1007/s12576-019-00678-5
11. Koryagina YuV, Nopin SV, Abutalimova SM, Ter-Akopov GN. Vegetative regulation of the heart rate of highly qualified ski racers in the conditions of training in the middle mountains. Problems of Balneology, Physiotherapy and Exercise Therapy. 2021;98(3–2):98 (In Russ.). https://doi.org/10.17116/kurort20219803221
12. Morphofunctional state of athletes with a history of covid-19 in the conditions of the middle mountains. Theory and practiceof physical culture. 2022;(12):33–5 (In Russ.). EDN: JDPFMX
13. Sperlich PF, Holmberg HC, Reed JL, Zinner C, Mester J, Sperlich B. Individual versus Standardized Running Protocols in the Determination of VO2max. J Sports Sci Med. 2015;14(2): 386–93. PMCID: PMC4424469
14. Bennett MH, Lehm JP, Jepson N. Hyperbaric oxygen therapy for acute coronary syndrome. Cochrane Database of Systematic Reviews. 2015.23(7);CD004818. https://doi.org/10.1002/14651858.cd004818.pub4 14. Branco BH, Fukuda DH, Andreato LV, Santos JF, Esteves JV, Franchini E. The Effects of Hyperbaric Oxygen Therapy on PostTraining Recovery in Jiu-Jitsu Athletes. PLoS ONE. 2016;11(3):e0150517. https://doi.org/10.1371/journal.pone.0150517
15. Sharma AP. Factors Affecting Sea-Level Performance Following Altitude Training in Elite Athletes. Journal of Science in Sport and Exercise. 2022;4(2):315–30. https://doi.org/10.1007/s42978-022-00198-6
16. Park HY, Hwang H, Park J, Lee S, Lim K. The effects of altitude/hypoxic training on oxygen delivery capacity of the blood and aerobic exercise capacity in elite athletes — a meta-analysis. J Exerc Nutrition Biochem. 2016;20(1):15–22. https://doi.org/10.20463/jenb.2016.03.20.1.3
About the Authors
G. N. Ter-AkopovRussian Federation
Essentuki
Y. V. Koryagina
Russian Federation
Essentuki
S. M. Abutalimova
Russian Federation
Essentuki
S. V. Nopin
Russian Federation
Essentuki
Y. V. Kushnareva
Russian Federation
Essentuki
Supplementary files
Review
For citations:
Ter-Akopov G.N., Koryagina Y.V., Abutalimova S.M., Nopin S.V., Kushnareva Y.V. Hyperbaric oxygenation for assisting recovery of athletes including those affected by COVID-19 under medium-altitude conditions. Extreme Medicine. 2024;26(3):71-76. https://doi.org/10.47183/mes.2024-26-3-71-76

















