Scroll to:
Morbidity, mortality, and lethality of the Russian population due to respiratory diseases for 2016–2021 and COVID-19 for 2020–2021
https://doi.org/10.47183/mes.2024-26-3-113-121
Abstract
Introduction. The impact of the epidemic circulation of the novel coronavirus respiratory infection on the Russian population in terms of morbidity, mortality and lethality from respiratory diseases (RD) and consequent social damage requires an in-depth study.
Objective. The study set out to compare the morbidity, mortality and lethality dynamics of the total population of the Russian Federation due to respiratory diseases (RD) in 2016–2021 and COVID-19 in 2020–2021.
Materials and methods. The study was based on official statistical information provided by the Ministry of Health of the Russian Federation, Russian Federal State Statistics Service and Russian Federal Service for the Oversight of Consumer Protection and Welfare on the morbidity and mortality of the population due to RD (codes J00-J98 in accordance with the International Statistical Classification of Diseases and Related Health Problems, 10th edition (ICD-10). The data for 2020–2021 are compared with the average morbidity and mortality rates of the Russian population for 2016–2019. Statistical data processing was carried out using Statistica software, version 10, and Epi5 (WHO), version 7. When comparing the indicators, the relative risk, 95% confidence interval, and Matel-Hansel2 were calculated. The differences were considered to be significant at p < 0.05.
Results. The primary and general morbidity and mortality from RD in the Russian population in 2020–2021 exceeded the average levels of similar indicators for 2016–2019. The increase in indicators was associated with a larger number of patients presenting with pneumonia, as well as interstitial and suppurative lung diseases. This was accompanied by an increase in hospital mortality and lethality due to RD and COVID-19 in 2020–2021.
Conclusions. The epidemic circulation of the new coronavirus infection was accompanied by a significant increase in the morbidity and mortality of the population from RD.
For citations:
Bilichenko T.N., Bystritskaya E.V., Misharin V.M. Morbidity, mortality, and lethality of the Russian population due to respiratory diseases for 2016–2021 and COVID-19 for 2020–2021. Extreme Medicine. 2024;26(3):113-121. https://doi.org/10.47183/mes.2024-26-3-113-121
INTRODUCTION
Respiratory diseases (RD) represent a widespread group of diseases affecting the Russian population, whose increasing incidence and differs significantly in the territories of cold and southern climatic zones having a different gender and age structure and population density [1]. The epidemic circulation of the new coronaviral infection COVID-19 had a great impact on the morbidity and mortality of the Russian RD population in 2020-2021, the significance of which requires in-depth study [2].
OBJECTIVE
To study the dynamics of morbidity, mortality and lethality rates of the total population of the Russian Federation due to respiratory diseases (RD) in 2016–2021 and COVID-19 in 2020–2021.
MATERIALS AND METHODS
We present an analysis of statistical data provided by the Ministry of Health of the Russian Federation and Russian Federal State Statistics Service on primary and total morbidity and mortality of the total population of the Russian Federation due to RD (class X J00-J99, according to the International Statistical Classification of Diseases and Related Health Problems, 10th edition (ICD-10) for 2016–2021 and morbidity COVID-19 (code U07.1, U07.2) [3–6]. The state statistical reporting forms No. 12 and No. 14 for 2019–2021 were used for the analysis. The data analysis was carried out using the statistical programs Statistica v.10, and Epi5 (WHO), v.7. The average indicators of overall incidence for 2016–2019 and the hazard ratio (HR) in 2020 and 2021 were calculated compared with the average value for previous years. When comparing the indicators, the difference p < 0.05 was considered significant. The data analysis was carried out by the following Federal Districts (FD) of Russia: Central (CFD); Northwestern (NWFD); Southern (SFD), North Caucasus (NCFD), Volga (VFD), Ural (UFD), Siberian (SFD), Far Eastern (FEFD), and the Crimean Federal District (which existed from 2014–2016).
RESULTS
According to the data of the Ministry of Health of the Russian Federation, a total of 59,731,931 cases of RD were registered in 2019, including 52,277,647 primary cases (87.5% of all RD) and 769,691 cases of secondary pneumonia (1.47% of all RD). By way of comparison, in 2020, these indicators increased to total RD 61,312,356 (+2.65%), 54,273,331 cases of primary infection (+3.82%) and 1,989,498 cases of pneumonia (+158.48%), while, in 2021, total RD amounted to 66,596,584 cases (+11.49%), including 59,381,887 cases of primary infection (13.59%) and 1,997,536 cases of pneumonia (+159.52%).
In 2021, the morbidity of the total population due to RD amounted to 45,560.7 cases per 100,000 of the total population, ahead of cardiovascular system diseases (24,792.3 cases), musculoskeletal system (12,087.0 cases), genitourinary system (10,591.0 cases), digestive system (10,332.9 cases).
Although the RD morbidity of the Russian total population has tended to increase since 2016, a significant increase in cases of diseases occurred in 2021. In terms of dynamics over the years since 2016, RD morbidity increased by 1% in 2017 (HR = 1.01; 95% CI 1.01–1.02; p < 0.001), by 3% in 2018 (HR = 1.03; 95% CI 1.02–1.03; p < 0.001), and by 2% in 2019 (HR = 1.02; 95% CI 1.01–1.02; p < 0.001). The average RD morbidity of the total population for 2016–2019 was 40,516.5 per 100,000. In 2020, the RD morbidity of the total population exceeded the 4-year average level to reach 41,862.9 and HR = 1.03; 95% CI 1.03–1.04; p < 0.001; in 2021 — 45,560.7 per 100,000 and HR = 1.12; 95% CI 1.12–1.13; p < 0.001 (Fig. 1). Morbidity of the total population in 2021 increased in all federal districts as compared with the levels of 2016–2019 with a maximum value in the Northwestern Federal District (Table 1). The excess of the average level of RD morbidity in Russia in 2021 was noted in 4 federal districts: SFD — 48,059.9 (HR = 1.05; 95% CI 1.05–1.06; p < 0.001); VFD — 49,837.3 (HR = 1.09; 95% CI 1.09–1.10; p < 0.001); UFD — 51 497.4 (HR = 1.13; 95% CI 1.13–1.13; p < 0.001); and NWFD — 55,680.9 (HR = 1.22; 95% CI 1.22–1.23; p < 0.001).
Among the subjects of the Russian Federation in 2021, the highest rates of RD were observed in the Nenets Autonomous District of the Northwestern Federal District (68,330.0 per 100,000 of the total population), the Chukotka Autonomous District of the Far Eastern Federal District (67,133.1), the Oryol Region of the Central Federal District (63,035.6), the Altai Territory of the SFD (64,924.9), the Vladimir Region of the Central Federal District (62,978.7), and the Republic of Sakha (Yakutia) of the Far Eastern Federal District (62,861,4).
Below-average RD morbidity for Russia in 2021 was experienced in the North Caucasus Federal District (33,292.3), Southern Federal District (37,185.5), Central Federal District (42,282.2), and Far Eastern Federal District (44,988.8). The lowest RD morbidity in the subjects of the Russian Federation in the North Caucasus Federal District was in the Chechen Republic (21,600.4 cases per 100,000 of the total population), the Kabardino-Balkarian Republic (24,874.5), and the Republic of Ingushetia (28,692.5).
The RD primary incidence rate (PIR) in the total population in 2016–2019 tended to increase: 2016 — 35,161.2; 2017 — 35,356.6 (HR = 1.01; 95% CI 1.00–1.01; p = 0.004); 2018 — 35,982,0 (HR = 1.02; 95% CI 1.02–1.03; p < 0.001); 2019 — 35,616.2 per 100,000 of the total population (HR = 1.01; 95% CI 1.01–1.02; p < 0.001). The average 4-year RD rate was 35,529.0 per 100,000 of the total population. In 2020, the RD index increased to 37,056.8 (HR = 1.04; 95% CI 1.04–1.05; p < 0.001); in 2021, to 40,624.9 per 100,000 of the total population (HR = 1.14; 95% CI 1.14–1.15; p < 0.001). In 2021, a higher than the average Russian indicator of the total population (40,624.9 per 100,000 of the total population) was registered in the NWFD — 49,744.0 (HR = 1.22; 95% CI 1.21–1.24; p < 0.001), UFD — 46,756.1 (HR = 1.15; 95%CI 1.14–1.16; p < 0.001), VFD — 44 786.8 (HR = 1.10; 95% CI 1.09–1.11; p < 0.001), SFD — 41 831.9 (HR = 1.03; 95% CI 1.02–1.04; p < 0.001). In 2021, the highest RD rates were recorded in the Nenets Autonomous District of the Northwestern Federal District (65,189.6), the Chukotka Autonomous District of the Far Eastern Federal District (63,589.6), the Vladimir Region of the Central Federal District (59,023.3), the Oryol Region of the Central Federal District (59,010.5 per 100,000 of the total population). The lowest RD rates were recorded in the Kabardino-Balkarian Republic (21,714.9 per 100,000 of the total population), the Republic of Ingushetia of the North Caucasus Federal District (20,131.4), the Chechen Republic of the North Caucasus Federal District (16,528.7).
In 2020, the COVID-19 disease of the total Russian population in terms of access to medical institutions was registered at the level of 3391.1 cases per 100,000 of the total population (4,966,644 people) with a 2.4–fold increase in the disease in 2021 — 8,085.7 cases per 100,000 of the total population (11,818,983 people). In 2021 The highest rates of COVID-19 were detected in the Northwestern Federal District (10,625.6), UFD (9,684.2), and Central Federal District (8,969.4 cases per 100,000 of the total population). In the Southern Federal District, the incidence of COVID-19 increased by 3.5 times: from 1835.3 in 2020 to 6386.3 cases per 100,000 of the total population in 2021. The highest incidence of COVID-19 in 2021 was registered in St. Petersburg (NWFD) at 13814.5 per 100,000 of the total population (74 3820 people), representing a 2.4-times increase compared to 2020 (5856.8 per 100,000 of the total population — 315 751 people). In Moscow (CFD), the incidence of COVID-19 was higher than the national average, but lower than in St. Petersburg: 2020 — 6191.0 cases per 100,000 (784,192 people); 2021 — 8976.0 cases per 100,000 of the total population (1,135,919 people), respectively.
COVID-19 incidences in the total population are below the national average in 2021. They were registered in the North Caucasus Federal District (3975.9), Southern Federal District (6386.3), Far Eastern Federal District (7295.3), VFD (7635.8), SFD (7913.3 cases per 100,000 of the total population). In terms of Russian Federal Subjects, the lowest rates of COVID-19 were detected in 2021 in the Chechen Republic of the North Caucasus Federal District at 1170.1 cases per 100,000 of the total population.
As well as pneumonia, acute laryngitis and tracheitis occupied a leading place in the structure of separate RD morbidity of the total population in 2021. Compared with the average level for 2016–2019 (2387.6 per 100,000 of the total population), the incidence of acute laryngitis and tracheitis of the total population in 2020 decreased to 2309.2 (HR = 0.97; 95%CI 0.95–0.98; p < 0.001) and in 2021 — 2215.2 (HR = 0.93; 95%CI 0.91–0.94; p < 0.001).
The incidence of pneumonia in the total population hardly differed 2016 and 2017, while in 2018 and 2019, an increase occurred: 2016 — 462.5 per 100,000 of the total population; 2017 — 457.7 (p = 0.49); 2018 — 514.6 (HR = 1.11; 95% CI 1.08–1.14; p < 0.001); 2019 — 524.4 (HR = 1.13; 95% CI 1.10-1.17; p < 0.001) (Table 2). Compared with the average level for 2016–2019 (489.7 per 100,000 of the total population), the incidence of pneumonia in 2020 and 2021 increased 2.8 times: 1358.4 (HR = 2.77; 95% CI 2.69–2.86; p < 0.001) and 1366.6 (HR = 2.79; 95% CI 2.70–2.88; p < 0.001), respectively. An increase in the incidence of pneumonia in 2020–2021 was noted in all territories of the Russian Federation with a maximum increase in the incidence of pneumonia in 2021 in the Southern Federal District, North Caucasus Federal District, VFD, and the Far Eastern Federal District.
Compared with the average level for 2016–2019 (1156.6 per 100,000 population), there was a decrease in 2020 and 2021 of chronic and unspecified bronchitis and lung emphysema in the total population (1092.1; HR = 0.74; 95% CI 0.72–0.75; p < 0.001) and 1055.3 cases (HR = 0.97; 95% CI 0.94–0.99; p = 0.008), respectively.
The average level of the total population for 2016–2019 of bronchial asthma (BA) was 1058.3; this did not significantly change in 2020 (1059.4; p = 0.936) and in 2021 (1073.1; p = 0.320).
Compared with the average level of chronic obstructive pulmonary disease (COPD) in the total population for 2016–2019. (562.3 per 100,000 of the total population) in 2020, the morbidity index decreased to 542.3 (HR = 0.96; 95% CI 0.94–0.99; p = 0.004) and did not change in 2021 — 529.3 (p = 0.065)
The average level of the total population for 2016–2019 with other interstitial pulmonary diseases, purulent and necrotic conditions of the lower respiratory tract, and other pleural diseases was 24.7 and did not change in 2020 (27.7 cases; p = 0.127), but increased in 2021 — 39.5 respectively (HR = 1.43; 95% CI 1.26–1.62; p < 0.001).
According to the data of statistical forms No. 14, in 2019, inpatient treatment for RD (J00-J98 ICD-10) was carried out in only 1,541,339 adult patients aged 18 and over, among whom 24,816 people died (1.6%). 252,105 people were treated in hospital for acute respiratory infections (ARI) of the upper respiratory tract (URT) (J00-J06 ICD-10); among these, 38 people died (0.02%); with lower respiratory tract infections (LRT) (J20-J22 ICD-10), 63,829 people were affected, of whom 7 people died (0.1%); pneumonia (J12-J18 ICD-10) — 439,901 people, 10,510 people died (2.39%).
Although in 2020, the number of patients aged 18 and over who received inpatient treatment for RD decreased, the lethality increased by 3 times. A total of 1,348,122 adult patients were discharged from hospitals, of whom 65,997 died (4.9%; p < 0.001): URT ARI– 172,366 people, 28 people died (0.02%) and LRT ARI– 45,333 people, 205 people died (0.45%; p < 0.001), pneumonia — 646,444 people, 47,939 people died (7.42%; p < 0.001).
In 2021, the number of patients aged 18 and over who received inpatient treatment for RD continued to decrease, but lethality among them increased mainly due to pneumonia. A total of 1,008,875 adult patients were discharged from hospitals, 64,909 people died (6.43%; p < 0.001), among whom URT ARI– 128,922 cases, 40 people died (0.03%) and LRT ARI — 45,333 cases, 205 people died (0.45%; p < 0.001); pneumonia — 378,715 cases, 48,711 died people (12.86 %; p < 0.001).
In connection with COVID-19 (U07.1-U07.2 ICD-10) in 2020, 1,902,903 people were discharged from hospitals at the age of 18 or more, among whom 1,154,77 people died (6.07%), 3,588,017 people were discharged in 2021, 458,529 people died (12.78%; p < 0.001).
Among children 0–17 years old in 2019, only 18,098 people were discharged from hospitals in connection with RD, 334 people (0.02%) died, including 779,103 people with ARI, 12 people (0.002%) died and LRT — 492,981 people, 10 people (0.002%) died; with pneumonia — 272,339 people, 226 people died (0.080%).
In 2020, there were only 1,095,976 children aged 0–17 in hospitals for RD, 313 people died (0.029%), among whom URT ARI– 469,594 people, 13 people died (0.003%) and LRT ARI — 314,116 people, 5 people died (0.002%); with pneumonia — 143,627 people, 213 people died (0.148%; p < 0.001).
In 2021, among children 0–17 years old, only 1,170,033 people were discharged from hospitals for RD. 339 people died (0.029%), among whom URT ARI — 508,705 people, 10 people died (0.002%) and LRT ARI — 333,031 people, 16 people died (0.005%; p < 0.001), 139,279 people died with pneumonia, 239 people died (0.171%; p < 0.001).
In connection with COVID-19 (U07.1–U07.2 ICD-10), 44,964 children were discharged from hospitals in 2020, of which 40 died — 0.090%. In 2021, 85,838 children were discharged, that is, 1.9 times more, of which 164 died (0.191%; p < 0.001).
Thus, the total number of RD patients discharged from hospitals in 2019 was only 3,341,437, 25,150 people died (0.75%), in 2020 — only 2,444,098 people, 66,310 people died (2.71%; p < 0.001), in 2021 — only 2,178,908 people, 65,248 people died (2.99%; p < 0.001).
In 2020, only 1,947,867 people with COVID-19 were discharged from hospitals, including 115,517 people (5.93%) died, in 2021 — only 3,673,855 people, 458,693 people died (12.48%; p < 0.001).
According to Russian Federal State Statistics Service, in the structure of mortality rates from all causes per 100,000 population in 2021 (1,673.9 cases) RD ranked 5th (78.7 cases — 4.7% of all cases) after diseases of the cardiovascular system (640.3 cases — 38.3% of all cases), mortality from COVID-19 (319.1 cases — 19.1% of all cases), neoplasms (194.1 cases — 11.6% of all cases), external causes (95.1 — 5.7% of all cases) [7].
If in the period 2016–2019 there was a decrease in RD mortality from 48.0 to 40.3 per 100,000 population (p < 0.001), then in the period 2020-2021 there was an increase in RD mortality of the total population of the Russian Federation (Fig. 2) [7–9].
The increase in RD mortality in 2020 compared to 2019 (40.3 cases per 100,000 of the total population) amounted to 72.46% (69.5%; p < 0.001); in 2021, the corresponding figure was 95.3% (78.7%; p < 0.001). An increase in the RD mortality of the population in 2020 and 2021 was noted in all territories of Russia, but above the average Russian level in 2021. Mortality was registered in the Volga Federal District (102.7 per 100,000 population), Far Eastern Federal District (111.0), SFD (93.1), and Southern Federal District (88.4 cases) (Table 3).
Below the average Russian level, the respiratory disease mortality rate was registered in the UFD (49.1), NWFD (55.8), Central Federal District (64.5), and North Caucasus Federal District (65.9 per 100,000 population). Among the subjects of the Russian Federation, the highest respiratory disease mortality rate in 2021 was recorded among the population of the Bryansk region of the Central Federal District (261.7 per 100,000 population). High respiratory disease mortality rates in 2021 were registered in the subjects of the Volga Federal District: the Kirov Region (256.3 per 100,000 population), the Republic of Mari El (231.8), the Republic of Bashkortostan (222.1), and in the Republic of Mordovia (114.5 per 100,000 population). The lowest respiratory disease mortality rate was registered in 2021 in Moscow Central Federal District (21.7), St. Petersburg NWFD (23.9), and Yamal-Nenets Autonomous District of the UFD (24.2 per 100,000 population).
The respiratory disease mortality rate had a direct relationship with age. In 2021, the respiratory disease mortality rate of the total population of the Russian Federation at the age of 0-17 years was 2.2; of the able–bodied population — 27.2; over the working age — 254.7 per 100,000 of the population of the corresponding age. The highest respiratory disease mortality rates were registered in the age group of 85 and older: in 2020 — 561.1, in 2021 — 713.0 per 100,000 population (the ratio of the level of 2021 to 2020 was 127.1%).
Among individual federal districts, the highest respiratory diseases mortality rate in 2021 were recorded in the Far Eastern Federal District: at the age of 0–17 years — 4.5; working–age population — 41.3; older than working age — 407.4 per 100,000 population of the corresponding age.
Among the subjects of the Russian Federation, the highest respiratory disease mortality rates are registered in the Republic of Bashkortostan of the Volga Federal District: 0–17 years old — 5.6; able–bodied population — 56.0; older than working age — 800.1 per 100,000 population of the corresponding age. The lowest mortality rates were registered in the Central Federal District of Moscow: among the total working-age population (6.4), older than the working age (66.6 of the corresponding age).
Among all men in 2020, the respiratory disease mortality rate was 84.5 per 100,000 male population (58,968 people); in 2021, it increased to 91.4 (64,155 people — +8.2%); p < 0.001. Among all women, the respiratory disease mortality rate in 2020 was 2.83 times lower than that of men, amounting to 29.9 (37,571 people), p < 0.001; in 2021, it was 2.36 times lower — 38.8 per 100,000 female population (50,572 people — +29.8%), p < 0.001. In 2021, among men of working age, the respiratory disease mortality rate was 3.2 times higher than among women (40.6 and 12.7, respectively, per 100,000 of the population of the corresponding age and gender; p < 0.001); in men older than working age, it was 2.4 times higher (431.2 and 179.4, respectively; p < 0.001). In 2021, the respiratory disease mortality rate of men of working age was higher than the average Russian level in the Far Eastern Federal District (59.5), CFD (50.0), VFD (49.9), SFD (43.4 per 100,000 of the corresponding age population). Below-average Russian mortality rates were recorded in the Northwestern Federal District (35.3), Central Federal District (34.0), UFD (27.8), and North Federal District (26.5 per 100,000 of the population of the corresponding age). In 2021, the respiratory disease mortality rate of women of working age above the national average was also registered in the Far Eastern Federal District (20.4), the SFD (16.6), the Volga Federal District (15.1), the Southern Federal District (15.1 per 100,000 population of the appropriate age); below average Russian mortality rates were recorded in the Northwestern Federal District (10.5), Central Federal District (9.8), North Caucasus Federal District (9.4), and UFD (8.3).
In the structure of the total RD mortality, the proportion of pneumonia mortal rate (J12-J16, J18) in 2021 was 65.3%. The levels of mortality rate from pneumonia in 2021 of the total population increased by 3.2 times compared to 2019 (16.3 per 100,000 villages): 2020 — 39.8 (p < 0.001); 2021 — 51.3 (p < 0.001) (Table 4). The increase in mortality from pneumonia in 2021 compared to 2020 has amounted to 28%. Above-national-average morality rates in 2021 were registered in the Far Eastern Federal District (81.9 per 100,000 population), the SFD (63.9), the VFD (66.5), the Southern Federal District (66.7 per 100,000 population), and the lowest mortality are in the UFD (21.7), Central Federal District (37.9), North Caucasus Federal District (38.6), Northwestern Federal District (41.8). Among the working-age population in 2021 The mortality from pneumonia was 20.3 per 100,000 of the population of the corresponding age. The highest mortality from pneumonia in this age group were recorded in the Far Eastern Federal District (33.9 per 100,000 population of the corresponding age), the SFD (25.6), the VFD (24.5), the Southern Federal District (23.0), while the lowest mortality rates were recorded in the UFD (11.3), the North Caucasus Federal District (12.6), the Central Federal District (15.8), and the Northwestern Federal District (19.8).
Mortality from COPD (J41, J42, J44) of the total population of the Russian Federation ranged from 22.5 in 2016 to 21.4 per 100,000 population in 2021 (p>0.05). In the structure of total RD mortality COPD mortality rate was 26.0%.
The bronchial asthma (J45-J46) mortality rate of the total population of the Russian Federation in 2021, which did not change, ranged from 1.0 per 100,000 population in 2016 to 0.8 in 2021 (p > 0.05).
In 2021, the contribution to the overall mortality structure of COVID-19 was 19.1%. Compared with 2020, there was a 3.2-fold increase in mortality rate due to COVID–19 in 2021 — from 98.8 (144,691 people) to 319.1 deaths (465,525 people) per 100,000 population (p < 0.001). An increased mortality rate from COVID-19 in 2021 was noted in all eight federal districts in 85 subjects of the Russian Federation. A higher mortality rate from COVID-19 than the average Russian level in 2021 was registered in the Northwestern Federal District (370.5), Central Federal District (367.7), UFD (355.1 deaths per 100,000 population). Among Russian Federal Subjects, the highest mortality rates from COVID-19 in 2021 occurred in the Orenburg region of the Volga Federal District — 472.6; Kursk region of the Central Federal District — 465.7; Oryol region of the Central Federal District — 460.9; Voronezh region of the Central Federal District — 460.4; Omsk region of the SFD — 448.1 per 100,000 population. Below average mortality rates from COVID-19 in 2021 were observed in the North Caucasus Federal District (156.1), Far Eastern Federal District (228.0), SFD (294.0), VFD (312.2), and Southern Federal District (314.9 deaths per 100,000 population). Among the Russian Federal Subjects, the lowest mortality rates from COVID-19 were noted in the Kirov Region of the Far Eastern Federal District — 65.2, the Chukotka Autonomous District of the Far Eastern Federal District — 76.3, the Republic of Tyva of the SFD — 99.6, the Chechen Republic of the North Caucasus Federal District — 103.2, and the Sakhalin Region of the Far Eastern Federal District — 106.4 per 100,000 population.
Compared to 2020, 2021 saw an increase in mortality from COVID-19 in all age groups, both among men and women. The highest mortality rates from COVID-19 were registered in the age group of 85 and older — 867.1 (2020) and 3052.93 deaths (2021) per 100,000 population, respectively.
Compared to 2020, the mortality from COVID-19 increased in 2021 among men by 2.7 times (from 107.3 to 286.1 deaths per 100,000 population, respectively; p < 0.001) and among women by 3.8 times (from 91.4 to 347.8 deaths per 100,000 population, respectively; p < 0.001). Moreover, if in 2020 mortality was higher in men, then in 2021 a higher mortality was recorded in women.
Among men in 2021, mortality rates due to COVID-19 above the national average (286.1 deaths per 100,000 population) were recorded in the Northwestern Federal District (344.0), Central Federal District (328.0), UFD (320.0), and Southern Federal District (287.9). The highest mortality rates from COVID-19 in men occurred in the Voronezh region of the Central Federal District (404.0 deaths per 100,000 population). Lower than the average Russian mortality rates due to COVID-19 in men were registered in the North Caucasus Federal District (146.4), Far Eastern Federal District (203.5), SFD (263.0), VFD (273.5 deaths per 100,000 population); the lowest mortality rate was recorded in the Kirov region of the VFD (61.5).
Among women in 2021, the mortality rate from COVID-19 was higher than the average in Russia (347.8 deaths per 100,000 population) in the UFD (385.8), Northwestern Federal District (393.2), Central Federal District (401.6). Mortality rates below the average were recorded in the North Caucasus Federal District (164.9), Far Eastern Federal District (251.1), SFD (321.1), Southern Federal District (338.3), and VFD (345.5). The highest mortality due to COVID-19 among women was registered in the Orenburg Region of the Far Eastern Federal District (533.2 deaths per 100,000 population), the Ivanovo Region of the Central Federal District (507.0); the lowest mortality rate from COVID-19 was recorded in the Chukotka Autonomous District of the Far Eastern Federal District (53.1).
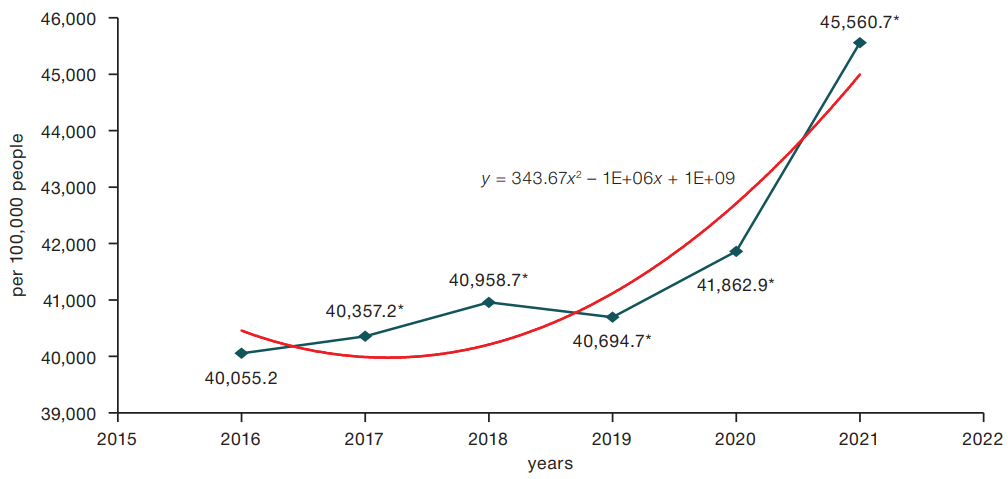
Figure prepared by the authors
Fig. 1. Dynamics of the general incidence of respiratory diseases in the total population in 2016–2021. (polynomial trend line. * — p < 0.05)
Table 1. Total incidence of respiratory diseases of the total population of the Russian Federation in 2016–2021
|
Territory |
Total RD incidence (per 100,000 people) |
|||||
|
Years |
||||||
|
2016 |
2017 |
2018 |
2019 |
2020 |
2021 |
|
|
RUSSIA |
40,055.2 |
40,357.2 |
40,958.7 |
40,694.7 |
41,862.9 |
45,560.7 |
|
CFD |
37,784.6 |
37,658.0 |
38,352.1 |
38,142.3 |
38,836.9 |
42,282.2 |
|
NWFD |
50,180.9 |
50,547.9 |
51,659.9 |
50,224.1 |
49,599.5 |
55,680.9 |
|
SFD |
33,226.2 |
33,260.5 |
33,611.4 |
34,363.1 |
34,518.4 |
37,185.5 |
|
NCFD |
30,420.8 |
30,699.6 |
29,334.1 |
30,423.9 |
32,300.6 |
33,292.3 |
|
VFD |
43,762.0 |
43,968.1 |
44,783.2 |
43,866.8 |
46,756.2 |
49,837.3 |
|
UFD |
41,861.3 |
42,623.3 |
44,326.8 |
44,460.8 |
46,504.5 |
51,497.4 |
|
SFD |
40,086.0 |
41,222.4 |
41,866.4 |
41,434.4 |
42,976.2 |
48,059.9 |
|
FEFD |
41,285.9 |
41,930.9 |
41,527.1 |
41,586.9 |
41,299.0 |
44,988.8 |
Table prepared by the authors
Table 2. Incidence of pneumonia of the total population of the Russian Federation in 2016–2021
|
Territory |
Total incidence of pneumonia (per 100,000 people) |
|||||
|
Years |
||||||
|
2016 |
2017 |
2018 |
2019 |
2020 |
2021 |
|
|
RUSSIA |
462.5 |
457.7 |
514.6 |
524.4 |
1358.4 |
1366.6 |
|
CFD |
375.7 |
382.1 |
430.8 |
414.2 |
1190.0 |
1336.8 |
|
NWFD |
470.7 |
471.9 |
514.9 |
452.7 |
1071.2 |
1358.4 |
|
SFD |
483.3 |
448.6 |
492.5 |
479.5 |
1119.7 |
1551.9 |
|
NCFD |
380.0 |
423.4 |
419.2 |
465.2 |
1535.2 |
1377.8 |
|
VFD |
509.3 |
529.7 |
579.7 |
575.2 |
1829.2 |
1391.8 |
|
UFD |
503.7 |
459.8 |
567.9 |
660.1 |
1178.2 |
1130.6 |
|
SFD |
520.4 |
484.4 |
557.8 |
609.6 |
1447.6 |
1336.9 |
|
FEFD |
558.4 |
526.3 |
647.7 |
749.2 |
1286.1 |
1418.9 |
Table prepared by the authors
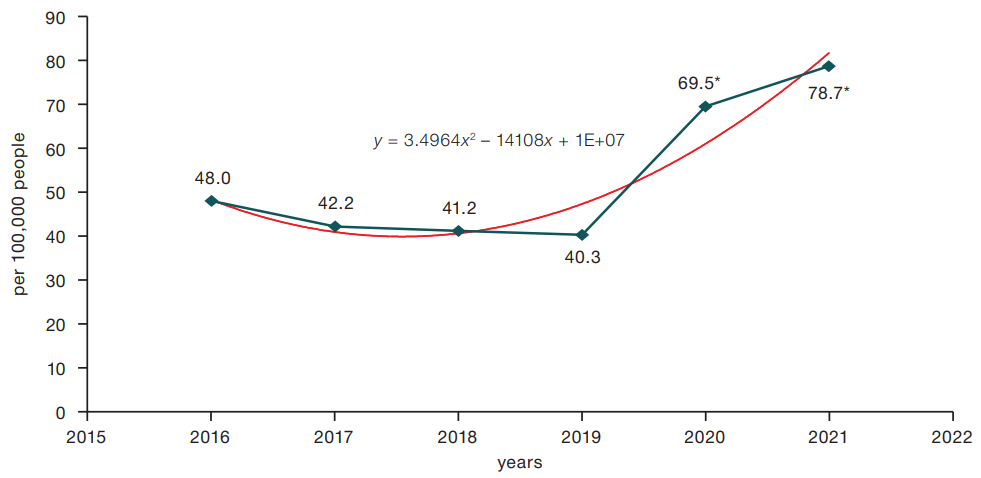
Figure prepared by the authors
Figure 2. Dynamics of mortality rates from respiratory diseases of the total population of the Russian Federation in 2016-2021. (Polynomial trend line. * — reliability of differences in indicators (p < 0.001)
Table 3. Mortality rates from the respiratory diseases of the total population in the federal districts of the Russian Federation in 2016–2021
|
Total respiratory diseases mortality rate (per 100,000 people) |
||||||
|
Territory |
Years |
|||||
|
2016 |
2017 |
2018 |
2019 |
2020 |
2021 |
|
|
RUSSIA |
48.0 |
42.2 |
41.6 |
40,3 |
65.9 |
78.7 |
|
CFD |
50.5 |
42.1 |
41.3 |
37.7 |
55.5 |
64.5 |
|
NWFD |
46.5 |
42.0 |
37.8 |
36.3 |
45.5 |
55.8 |
|
SFD |
36.6 |
32.0 |
33.6 |
35.7 |
59.1 |
88.4 |
|
NCFD |
32.5 |
30.7 |
27.7 |
28.0 |
72.9 |
65.9 |
|
VFD |
49.3 |
44.0 |
44.7 |
43.7 |
84.1 |
102.7 |
|
UFD |
44.7 |
39.8 |
34.8 |
30.2 |
52.2 |
49.1 |
|
SFD |
59.7 |
55.6 |
55.4 |
54.7 |
81.9 |
93.1 |
|
FEFD |
52.7 |
44.0 |
53.2 |
57.0 |
78.8 |
111.0 |
Table prepared by the authors
Table 4. Mortality rates from pneumonia of the total population in the federal districts of the Russian Federation in 2016-2021
|
Total pneumonia mortality rate (per 100,000 people) |
||||||
|
Years |
||||||
|
Territory |
2016 |
2017 |
2018 |
2019 |
2020 |
2021 |
|
RUSSIA |
21.3 |
17.8 |
17.5 |
16.3 |
39.8 |
51.3 |
|
CFD |
22.2 |
17.0 |
16.9 |
14.8 |
31.2 |
37.9 |
|
NWFD |
30.9 |
27.0 |
23.2 |
21.5 |
31.2 |
41.8 |
|
SFD |
19.3 |
15.5 |
16.1 |
18.1 |
41.0 |
66.7 |
|
NCFD |
6.4 |
4.7 |
4.9 |
5.6 |
45.9 |
38.6 |
|
VFD |
17.2 |
15.1 |
15.6 |
12.7 |
48.8 |
66.5 |
|
UFD |
16.6 |
13.9 |
10.5 |
8.3 |
25.6 |
21.7 |
|
SFD |
26.8 |
24.4 |
26.5 |
25.4 |
52.0 |
63.9 |
|
FEFD |
34.6 |
28.3 |
26.1 |
29.5 |
49.5 |
81.9 |
Table prepared by the authors
DISCUSSION
The presented analysis of official statistics from the Ministry of Health of the Russian Federation and Russian Federal State Statistics Service shows that during the epidemic circulation of the COVID-19 virus infection in 2020–2021, there was a significant increase in morbidity, hospital lethality and mortality of the total Russian population due to RD, in which structure pneumonia occupied a leading place. Compared to 2019, RD increased in the total population by 13.59% in 2021; pneumonia — by 159.52%, and RD — by 11.49%. Due to the conversion of hospitals for the treatment of patients with COVID-19, the number of patients hospitalized for RD decreased in 2020 and 2021; however, the severity increased, which led to a 3.97-fold increase in lethality from these diseases. Thus, the number of patients discharged from hospitals for RD in 2019 amounted to 3,341,437 people (lethality — 0.75%); in 2020 — 2,444,098 people (lethality — 2.71%); in 2021 — 2,178,908 people (lethality — 2.99%). The main contribution to the lethality rate of the population aged 18 and over was made by pneumonia (J12-J18 ICD-10): 2019 — 439,901 people (10,510 people died — 2.39%); 2020 — 646,444 people (47,939 people died — 7.42%); 2021 — 378,715 cases (48,711 people died — 12.86%). A similar situation of increased lethality from pneumonia was noted among children aged 0–17 years: 2019 — 272,339 people (226 people died — 0.08%); 2020 — 143,627 people (213 people died — 0.148%); 2021 — 139,279 people (239 people died — 0.171%).
In 2020, in Russia, the incidence of COVID-19 of the total population in terms of access to medical institutions was registered at the level of 3391.1 cases per 100,000 of the total population (4,966,644 people). This increased by 2.4 times in 2021 — 8,085.7 cases per 100,000 of the total population (11,818,983 people). In 2020 1,947,867 people were discharged from hospitals with COVID-19, which amounted to 39.22% of all patients with COVID-19 (lethality — 5.93%); in 2022, 1.89 times more — 3,673,855 people, that is, 31.08% of all patients with COVID-19 (lethality — 12.48%).
There were significant fluctuations in the levels of morbidity, overall incidence and lethality from RD in the population of different territories of the Russian Federation and age groups. As in the previous period, the highest incidence of RD in the population in 2020–2021 was recorded in the territories of the cold climate zone in the Northwestern Federal District, VFD, UFD, and SFD. The incidence of pneumonia among the population was higher than the national average in 2021. It was registered in the Southern Federal District, the North Caucasus Federal District, the Far Eastern Federal District and the Far Eastern Federal District.
During the COVID-19 epidemic in 2020-2021, there was an increase in RD mortality compared to 2019 (40.3 cases) by 72.46% in 2020 (69.5 cases), and in 2021 — by 95.3% (78.7 cases per 100,000 of the total population). Above average Russian levels of RD mortality in 2021 were registered in the Far Eastern Federal District (111.0), the Volga Federal District (102.7), the SFD (93.1), the Southern Federal District (88.4 cases per 100,000 population). RD mortality increased with age and was higher among men than among women. In the structure of mortality from all RD, mortality from pneumonia (J12-J16, J18) in 2021 was 65.3%. Mortality from pneumonia in the total population increased 3.2 times from 2019 (16.3) to 2021 (51.3 per 100,000 population). While etiological verification of pneumonia in 2020–2021 involves practical difficulties, given the data on the circulation of a novel coronavirus infection, it can be assumed that a significant part of it is associated with a previous viral infection.
In 2021, the highest incidence rates of COVID-19 were detected in the Northwestern Federal District (10,625.6), UFD (9684.2), Central Federal District (8969.4 cases per 100,000 of the total population) and mortality from COVID-19 in 2021 were also registered in the population of the same territories of the Northwestern Federal District, Central Federal District, UFD.
The problem of the epidemic circulation of the new coronavirus and the long-term course of the consequences of COVID-19 has posed new challenges that remain relevant for the healthcare system and the medical community at the present time. The severe course of COVID-19 is accompanied by multi-systemic manifestations of the disease involving an increase in mortality [2]. In this regard, improving the methods of primary prevention and effective treatment of COVID-19 and other respiratory infections will be of great importance for public health. The development and widespread introduction of a domestic vaccine against the new coronavirus since January 2021 made it possible to stop the epidemic and reduce mortality from COVID-19 in 2022. At the same time, the circulation of the new SARS-CoV-2 coronavirus continues along with other respiratory infections. The study of data on vaccination of Russia against influenza and pneumococcal infection in Moscow confirms the need for wider coverage of these methods of prevention of the population having a high risk of morbidity and mortality from respiratory infections [10]. A study of the risk factors for deaths in the adult population with COVID-19 based on the presented data showed that elderly, male patients had the highest risk. This is consistent with the results of foreign studies conducted on large groups of patients. Data on primary care of the electronic healthcare platform of England (OpenSAFELY), which covered 40% of all patients, were analyzed. Data from 17,278,392 adults were compared with data from 10,926 patients who died from COVID-19. They confirmed that old age increases HR = 1.59 by 10 years (95% CI 1.19–2.13), as well as male gender — HR = 1.59 (95% CI 1.53-1.65), belonging to black peoples — HR = 1.48 (95% CI 1.30–1.69) and South-Asian peoples — HR = 1.44 (95% CI 1.32-1.58) [11]. In older patients, chronic diseases that increase the risk of death are more common: coronary heart disease — HR = 5.16 (95% CI 5.16-8.49), chronic renal failure — HR = 3.69 (95%CI 3.09–4.39), COPD — HR = 3.55 (95% CI 1.88-6.79), obesity with BMI of 40 and above — HR = 1.92 (95% CI 1.72–2.13), diabetes mellitus — HR = 1.92 (95% CI 1.48–2.48), arterial hypertension — HR = 1.09 (95%CI 1.05–1.14) and other diseases [12]. According to the results of a comparative analysis of the data of 12,007 patients (10,761 with favorable and 1,246 with unfavorable COVID–19 outcomes) from 66 hospitals in the Moscow region, it was found that in the absence of comorbid conditions, the death rate was 9.4%; with one comorbid condition — 13.9% (p < 0.001); with multimorbidity — 24.8% (p < 0.001) [13].
Smoking at the time of the disease also increased the incidence of an adverse outcome (HR = 1.07; 95%CI 0.98-1.18) [12]. The adult population of Russia is characterized by a high prevalence of smoking among both men and women [14]. With the exception of the North Caucasus Federal District, the prevalence of smoking among men in other federal districts of Russia in 2021 exceeded 35.8%. Among women, the prevalence of smoking is higher than the national average (9.2%) registered in the Northwestern Federal District (12.6%), the UFD (11.4%), the SFD (12.7%) and the Far Eastern Federal District (18.9%), whose population is characterized by high incidence of acute and chronic RD.
Representing one of the strategic directions of medical science, pulmonology actively uses innovative methods of diagnosis and treatment in order to preserve the health of the Russian population [13]. The development and implementation of scientifically based RD prevention measures will help reduce morbidity and mortality, increase the duration of socially active life, and reduce the economic burden on the state due to RD.
CONCLUSIONS
- Compared with 2019, the total RD morbidity of the total population of Russia in 2021 increased by 11.49%, while the RD morbidity of the total population increased by 13.59%, mainly due to the increased incidence of pneumonia. Excesses in the average level of RD morbidity in Russia in 2021 were noted in four federal districts: SFD, VFD, UFD and NWFD.
- Due to the increase in the number of patients with COVID-19, hospitalization due to RD decreased in 2020 and 2021; however, the severity of infections increased, leading to a 3.97-fold increase in lethality from RD, primarily from pneumonia.
- In the period 2020–2021, there was an increase in RD mortality compared to 2019 by 72.46% in 2020 (69.5 cases), and in 2021 — by 95.3% (78.7 cases per 100,000 of the total population). Excesses of the average Russian level of RD mortality in 2021 were registered in the Far Eastern Federal District, VFD, CFD, and SFD.
- RD mortality increased with age and was higher among men than among women; however, in 2021, higher mortality rates among women were recorded. In the structure of mortality from all RD, the share of mortality from pneumonia (J12-J16, J18) in 2021 was 65.3%. Mortality from pneumonia in the total population increased 3.2 times from 2019 (16.3) to 2021 (51.3 per 100,000 population).
- The COVID-19 epidemic in 2020–2021, which was caused by the novel coronavirus SARS-CoV-2, had a significant impact on the morbidity and lethality of the Russian population from RD.
- The incidence of COVID-19 increased from 3,391.1 cases per 100,000 of the total population (4,966,644 people) in 2020 to 8,085.7 cases (11,818,983 people) in 2021, exceeding the national average in the UFD, Central Federal District, and Northwestern Federal District.
- An increase in mortality from COVID-19 in 2020–2021 was registered in all Federal districts of the Russian Federation; moreover, if in 2020 the mortality of men was higher, then in 2021 mortality was higher for women. Excesses in the average Russian mortality from COVID-19 in 2021 were recorded in the Northwestern Federal District, Central Federal District, and UFD.
- The increase in mortality from COVID-19 in 2021 was noted in all age groups; however, the highest levels were recorded in patients over the age of 85: among men — 2.7 times; among women — 3.8 times.
- Due to the continuing circulation of a novel coronavirus infections among the Russian population at the same time as other respiratory diseases, it is necessary to develop a program for the prevention of RD.
References
1. Bystritskaya EV, Bilichenko TN. The morbidity, disability and mortality associated with respiratory diseases in the Russian Federation in 2015-2019. Pul’monology. 2021;31(5):551–61 (In Russ.). https://journal.pulmonology.ru/pulm/article/view/2875
2. Bilichenko TN. Epidemiology of Coronavirus disease 2019 (COVID-19). Academy of medicine and sports. 2020;1(2):14–20 (In Russ.) https://doi.org/10.15829/2712-7567-2020-2-15
3. The incidence of the entire population of Russia in 2021 with a diagnosis established for the first time in life: Statistical materials. Moscow; 2022. Part. I.
4. The incidence of the entire population of Russia in 2016, 2017, 2018, 2019: Statistical materials. Moscow; 2017, 2018, 2019, 2020. Part II.
5. Total morbidity of the adult population of Russia in 2021: Statistical materials. Moscow; 2022. Part IV.
6. Medical and demographic indicators of the Russian Federation. 2021: Statistical materials. Moscow; 2022.
7. Federal State Statistics Service. Demographic yearbook of Russia. 2017; Available at: https://rosstat.gov.ru/storage/mediabank/Dem_ejegod-2017.pdf
8. Federal State Statistics Service. Demographic yearbook of Russia. 2019; Available at: https://rosstat.gov.ru/storage/mediabank/Dem_ejegod-2019.pdf.
9. Federal State Statistics Service. Demographic yearbook of Russia. 2022; Available at: https://rosstat.gov.ru/storage/mediabank/Ejegodnik_2022.pdf
10. Gruzdeva OA, Bilichenko TN, MA Baryshev, AV Zhukova. The impact of vaccination against influenza and pneumococcal infection on the incidence of acute respiratory viral infections and community-acquired pneumonia in the Central Administrative District of Moscow. Epidemiology and Vaccinal Prevention 2021; 20(2):28–41. https://doi.org/10.31631/2073-3046-2021-20-2-28-41
11. Williamson EJ, Walker AJ, Bhaskaran K, et al. Open SAFELY: factors associated with COVID-19 death in 17 million patients. Nature. 2020;584:430–6. https://doi.org/10.1038/s41586-020-2521-4
12. Molochkov AV, Karateev DE, Ogneva EYu, Zulkarnaev AB, Luchikhina EL, Makarova IV, Semenov DYu. Comorbidities and predicting the outcome of COVID-19: the treatment results of 13,585 patients hospitalized in the Moscow Region. Almanac of Clinical Medicine. 2020;48(S1):S1–10 (In Russ.). https://doi.org/10.18786/2072-0505-2020-48-040
13. Federal’naya sluzhby gosudarstvennoj statistiki Rossijskoj Federacii. Vyborochnoe nablyudenie sostoyaniya zdorov’ya naseleniya. Accessed July 07, 2022 (In Russ.).
14. Bilichenko TN, Shutov AA. The achievements of pulmonology and the main directions of further improvement of medical care to the population of the Russian Federation. Pulmonology. 2021;31(6):782–91 (In Russ.). https://doi.org/10.18093/0869-0189-2021-31-6-782-791
About the Authors
T. N. BilichenkoRussian Federation
Moscow
E. V. Bystritskaya
Russian Federation
Moscow
V. M. Misharin
Russian Federation
Moscow
Supplementary files
Review
For citations:
Bilichenko T.N., Bystritskaya E.V., Misharin V.M. Morbidity, mortality, and lethality of the Russian population due to respiratory diseases for 2016–2021 and COVID-19 for 2020–2021. Extreme Medicine. 2024;26(3):113-121. https://doi.org/10.47183/mes.2024-26-3-113-121
















