Scroll to:
Effectiveness of conservative methods for plantar fasciitis treatment in athletes
https://doi.org/10.47183/mes.2025-270
Abstract
Introduction. Plantar fasciitis (PF) is a multifactorial pathology that restricts an athlete’s training and competitive activities, leading to premature termination of a sports career in some cases. The search for optimal conservative treatment methods that may improve the overall therapy effectiveness represents an important task of sports medicine.
Objective. Development of a differentiated approach to conservative treatment of athletes suffering from PF, taking the biomechanical features of the disease into account.
Materials and methods. The study involved 82 athletes, including 37 men and 45 women suffering from unilateral PF with a median age of 30 (23; 34) years. The participants were divided into four groups depending on the type of therapeutical action: Group 1 — shock wave therapy (ESWT); Group 2 — vibration therapy combined with myofascial release of the muscles of the posterior thigh and shin; Group 3 — individual orthoses of the feet; Group 4 — a combination of vibration therapy, myofascial release, individual orthoses of the feet. The tested therapeutic measures were assessed by the dynamics of pain syndrome, the results of baropodometry, the severity of tension in the thigh and shin muscles, and changes in the thickness of plantar aponeurosis.
Results. All the studied treatment methods showed varying degrees of effectiveness in reducing pain (p < 0.001), reducing the thickness of plantar aponeurosis (p < 0.05), normalizing plantar pressure in the posterior and anterior parts of the affected foot (p < 0.05), and increasing the postural stability of athletes according to objective indicators (p < 0.05). The use of ESWT resulted in the most pronounced reduction in pain. In Groups 2 (vibration therapy and myofascial release) and 3 (individual foot orthoses), a statistically significant decrease in muscle tension in the posterior shin group was observed (p < 0.05). In addition, in Group 2, the angle of dorsiflexion of the ankle joint increased significantly (p < 0.05). Group 4 (combined treatment) demonstrated the highest level of biomechanical stability.
Conclusions. ESWT demonstrates a high effectiveness in relieving a pronounced acute process. In cases where an athlete experiences some biomechanical disorders or deformities of the foot, orthoses of the feet are advisable. In case of tension of the shin muscles and limitation of dorsiflexion, vibration therapy combined with myofascial release is recommended.
Keywords
For citations:
Slivin A.V., Karmazin V.V., Shlykov K.A., Parastaev S.A. Effectiveness of conservative methods for plantar fasciitis treatment in athletes. Extreme Medicine. 2025;27(1):115-123. https://doi.org/10.47183/mes.2025-270
INTRODUCTION
Plantar fasciitis (PF) is an urgent and widespread problem in sports that hinders the training process. Both conservative and surgical methods of treatment can be used to treat this pathology [1]. However, due to the prolonged recovery period and postoperative complication risks, conservative methods are recognized as the first line of therapy in clinical practice [2].
It has been repeatedly noted that the main problem faced by a physician in the treatment of athletes with PF is the low effectiveness of conservative interventions, including insufficient duration of pain relief [3]. Conservative treatment methods widely employ approaches of physical and rehabilitation medicine; however, none of the available PF treatment methods have been supported by convincing scientific evidence [4]. This may be related to biomechanical disorders underlying the development of degenerative changes in plantar aponeurosis, thus resulting in a significant heterogeneity of treatment outcomes.
Despite the wide range of correction methods tested in PF, including athletes, an integrated approach to combining therapeutical measures is yet to be developed. Tools for monitoring the effectiveness of therapeutic effects and tactics for managing athletes with PF should be improved in order to correct not only pain syndrome, but also to prevent disease recurrence.
In this connection, the assessment of disease risk factors and impaired biomechanical patterns is extremely important for PF in general and among athletes in particular [5]. The impact on key steps in the pathogenesis of the disease will make it possible to personalize therapeutical approaches and, accordingly, improve the outcome of therapeutic effects, and reduce the rehabilitation time for athletes.
In this study, we set out to develop a differentiated approach to the conservative treatment of athletes suffering from PF, taking the biomechanical features of the disease into account.
MATERIALS AND METHODS
The study included 82 athletes (37 men and 45 women) representing various sports: athletics, football, basketball, rugby, tennis, handball, volleyball, bobsleigh, fencing, and some others (Fig. 1). The median age of athletes was 30 (23; 34) years. The athletes underwent rehabilitation treatment at the Federal Research and Clinical Center of Sports Medicine and Rehabilitation during the 2023–2024 period.
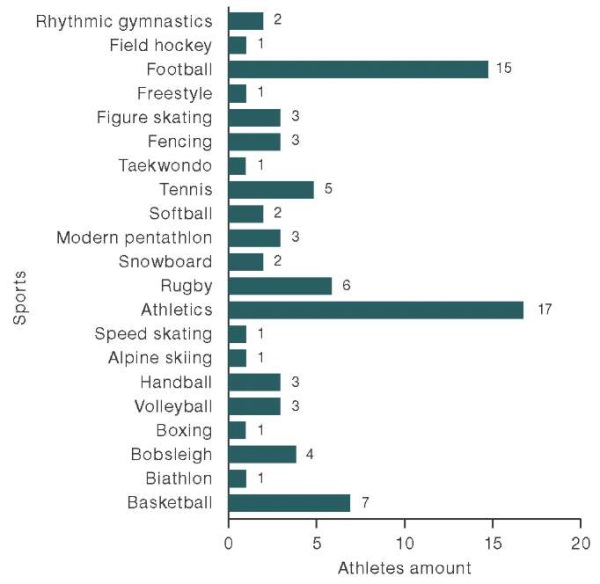
Figure prepared by the authors using their own data
Fig. 1. PF prevalence in various sports in the research sample
The criteria for inclusion in the study were: clinical diagnosis of PF with unilateral localization of the process, age from 16 to 50 years, presence of sports qualifications. Criteria for non-inclusion of athletes in the study were: excluded diagnosis of plantar fasciitis, presence of systemic connective tissue diseases, age that does not meet the inclusion criteria (less than 16 years and more than 50 years), inability to perform diagnostic and correction programs due to circumstances beyond their control (severe injuries, diseases, epidemic risks leading to interruption of a sports career), lack of athletic qualifications, refusal to participate in the study. Criteria for exclusion of athletes from the study were: injury to the musculoskeletal system that occurred during the study period, refusal to further participate in the study.
All athletes with PF were divided into four groups depending on the type of therapeutic measures performed:
- Group 1 (n = 27) — athletes who were treated with extracorporeal shock wave therapy (ESWT);
- Group 2 (n = 20) — athletes who were treated with vibration therapy combined with myofascial release (MFR) of the muscles of the posterior thigh and shin;
- Group 3 (n = 19) — athletes who underwent treatment using individual orthoses of the feet;
- Group 4 (n = 16) — athletes who were treated with vibration therapy combined with MFR of the muscles of the posterior thigh and shin, as well as with the use of individual orthoses.
Focused ESWT was performed on a BTL-6000 FSWT device (UK) with an energy flow area of 0.65 мJ/mm² and a frequency of 4–6 Hz. A course vibration exposure lasting 9–10 days was performed on a Vibrosphere device (Sweden) with a sequential increase in the frequency range from 20 to 45 Hz. The myofascial release of the muscles of the posterior thigh and shin was carried out by athletes independently using a roll with a ribbed surface. For the manufacture of individual orthopedic insoles, Formthotics blanks (New Zealand) were used.1
The effectiveness of curative services was assessed by the dynamics of pain syndrome, determined using the Russian version of the Visual Analog Scale Foot and Ankle — VAS FA [6]; the muscle pain in the posterior thigh and shin; evaluation of ankle joint range of motion by the angle of ankle joint dorsiflexion; baropodometry (in static and dynamic tests); and changes in the thickness of the plantar fascia. The muscle tenderness of the posterior thigh and shin was palpated, and the angle of ankle joint dorsiflexion was measured in a supine position with the knee joint extended by goniometry. Baropodometry was performed using the WINTRACK hardware and software complex (Medicaptures, France) according to an algorithm consisting of static and a series of dynamic tests (sagittal, frontal, forefoot lifting and jumping tests) [7]. In addition, changes in the center of pressure (CoP) velocity in the frontal and sagittal planes, as well as the statokinesiogram area, were evaluated: the CoP velocity in the frontal plane was evaluated in the sagittal dynamic test, and in the sagittal plane — in the frontal test; the statokinesiogram area was studied in the jumping dynamic. The thickness of the plantar fascia was determined using magnetic resonance imaging, which was performed on a SIGNA Creator installation 1.5 T (General Electric, USA). The measurement was performed on sagittal sections 1 cm distal to the place of attachment to the calcaneal protuberance. The effectiveness of curative services was evaluated after 7 and 14 days. On day 28 after the completion of curative services, an additional reassessment of the pain severity was performed. As an additional method for determining the presence and severity of foot pronation, the foot posture was assessed using the FPI-6 scale (Foot Posture Index — 6).
Statistical data analysis was carried out using the IBM SPSS Statistics 23 application software package. To assess the type of distribution of quantitative feature values, the Kolmogorov–Smirnov and Shapiro–Wilk criteria with a critical significance level of 0.05 were used. In the case of differences in the distribution from the normal, nonparametric analysis methods were applied. Descriptive statistics of quantitative data are given in the form of medians and quartiles; descriptions of qualitative features are given in the form of relative frequencies and their confidence intervals. The nonparametric Mann–Whitney U-test was used for comparative intergroup analysis; the Wilcoxon test was used for intragroup analysis. A comparison of discrete quantities was carried out using the χ² criterion. The significance level for all calculations of less than 0.05 was taken to be statistically significant.
RESULTS
The largest number of PF cases was observed in athletes involved in athletics, football, basketball, rugby, and tennis (Fig. 1). More detailed information about the study groups evaluated before the onset of curative services is presented in Table 1.
Table 1. Summary of athletes’ characteristics in groups before the onset of therapeutical measures
|
Parameter |
Group 1 (n = 27) |
Group 2 (n = 20) |
Group 3 (n = 19) |
Group 4 (n = 16) |
|
Age, years |
31 (23; 37) |
27.5 (24; 35) |
27 (21; 36) |
30 (25; 33) |
|
Body mass index, kg/m² |
22.1 (21; 23) |
21.8 (21; 24) |
22.2 (21; 24) |
22.8 (21; 25) |
|
Sports experience, years |
22 (18; 30) |
20 (17; 25) |
19 (16; 25) |
20.5 (17; 22) |
|
Pronation degree, FPI-6 score |
6 (5; 7) |
6 (4; 7) |
6 (5; 6) |
6 (5; 7) |
|
Ankle joint dorsiflexion angle, degree (°) |
15 (12; 18) |
20 (17; 23) |
19 (15; 22) |
19 (17; 22) |
Table prepared by the authors using their own data
Note: the data is presented as a value median (Mе) of the lower and upper quartiles Q [ 25–75%].
The study did not reveal any statistically significant differences in the sample by age, BMI, and sports experience. An assessment of the pronation degree on the FPI-6 scale found that the foot of athletes with PF was moderately pronated, with all the studied groups of athletes being comparable in this parameter.
Group 1, i.e., the athletes treated with ESWT, showed the lowest angle of ankle joint dorsiflexion, amounting to 15°. This indicates a more pronounced tension of the shin triceps muscle compared to other groups before the onset of curative services.
The analysis of the pain syndrome assessed by VAS FA revealed a statistically significant (p < 0.001) decrease in the pain syndrome intensity in all the studied groups in the follow-up period during the intragroup analysis. The corresponding data is shown in Fig. 2. Thus, in Group 1, the athletes reported a decrease in pain by 63%, in Group 2 — by 14%, in Group 3 — by 61%, and in Group 4 — by 18%. In the follow-up observation of athletes with PF, no statistically significant decrease in the VAS FA score was observed 28 days after the completion of therapy, which indicates the stability of the achieved therapeutic effect.
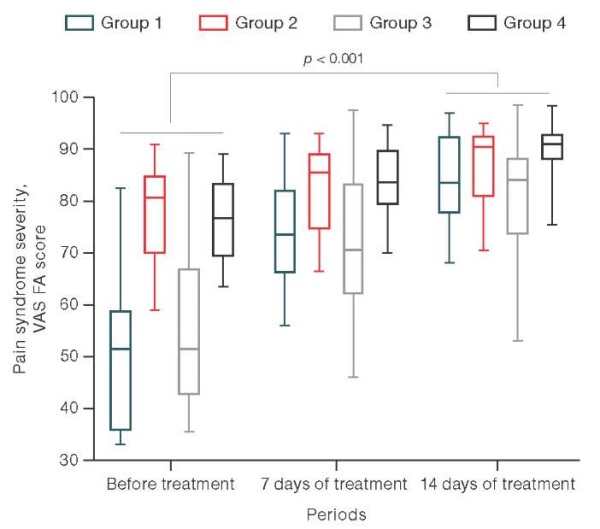
Figure prepared by the authors using their own data
Fig. 2. Effectiveness of curative services in athletes with PF by VAS FA pain assessment
In all the studied groups, an evaluation of the effectiveness of curative services found no statistically significant decrease in muscle tenderness of the posterior thigh group on palpation on days 7 and 14 of therapy compared with the period before the onset of the study. The corresponding data is shown in Fig. 3A.
At the same time, athletes from Groups 2, 3, and 4 showed a statistically significant decrease in tenderness and tension of the posterior shin muscles on palpation after 14 days compared with the period before treatment by 63%, 59%, and 61%, respectively (p < 0.05). The corresponding data are shown in Fig. 3B.
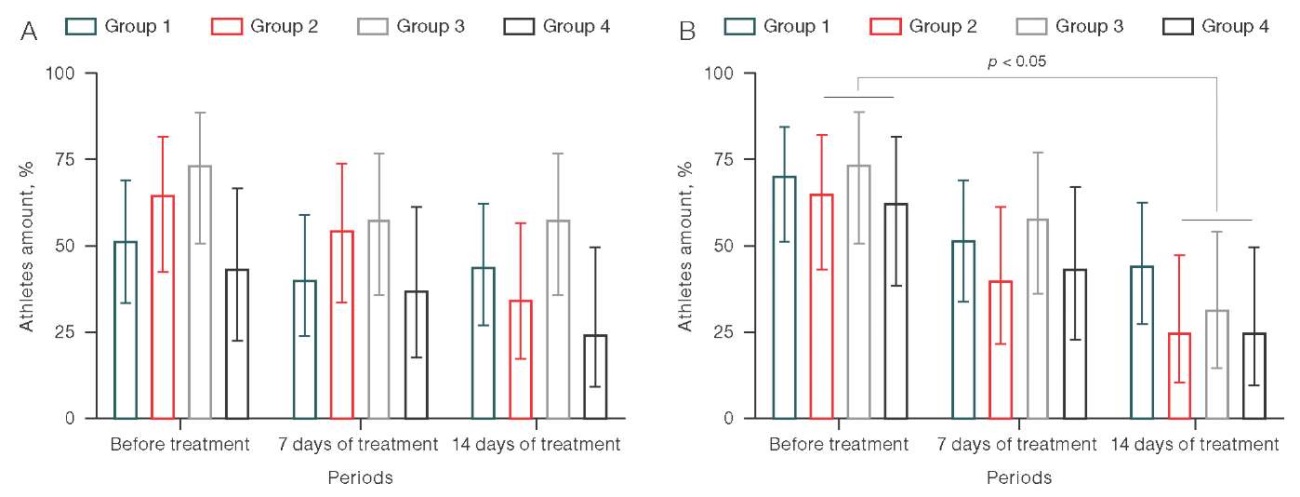
Figure prepared by the authors using their own data
Fig. 3. Effectiveness of therapeutic measures in athletes with PF by parameters
Note: A — muscle tenderness of the posterior thigh group; B — muscle tenderness of the posterior shin group.
In an intragroup analysis of changes of ankle joint dorsiflexion angle in follow-up (prior to treatment/14 days of treatment), athletes showed a statistically significant increase in the ankle joint range of motion in Groups 2 (vibration therapy and myofascial release) (p < 0.05) and 4 (vibration therapy, myofascial release, and individual foot orthoses) (p < 0.01) by 15% and 26%, respectively. No statistically significant dynamics was observed in other study groups (Fig. 4).
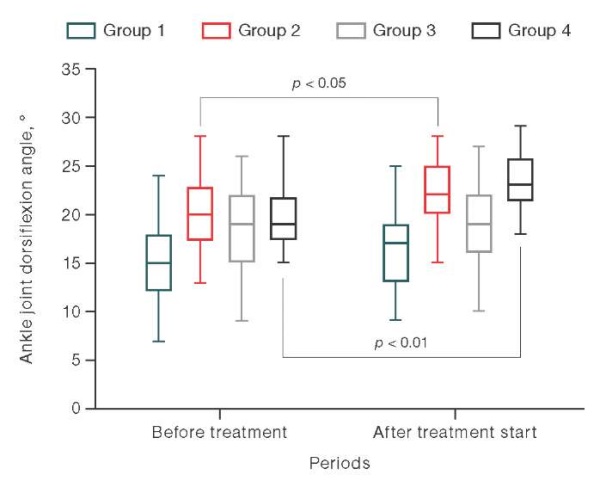
Figure prepared by the authors using their own data
Fig. 4. The effectiveness of curative services in athletes with PF by the ankle joint dorsiflexion angle
Table 2 presents the analysis of changes in plantar pressure on the support surface in the anterior and posterior parts of the affected foot before/after treatment according to baropodometry. During corrective actions, athletes in all groups showed normalization of the distribution of plantar pressure in the static test (p < 0.05). At the same time, in Groups 1 (ESWT) and 3 (individual orthoses of the feet), an increase in the pressure of the posterior part of the affected foot was detected by 37% and 18%, respectively. At the same time, Groups 2 (vibration therapy and myofascial release) and 4 (vibration therapy, myofascial release, and individual orthoses of the feet), conversely, showed a decrease in plantar pressure by 17% and 13%, respectively, compared to the measurements prior to treatment.
Table 2. Intragroup analysis of changes in plantar foot pressure in athletes with PF in various groups
|
Athlete groups |
Anterior part, % |
р |
Posterior part, % |
р |
||
|
before treatment |
after treatment |
before treatment |
after treatment |
|||
|
Group 1 (n = 27) |
27 (24; 29) |
24 (23; 24) |
<0.001 |
19 (14; 21) |
26 (23; 27) |
<0.001 |
|
Group 2 (n = 20) |
20.5 (17; 23) |
23 (22; 24) |
0.001 |
35 (29; 39) |
29 (27; 31) |
0.001 |
|
Group 3 (n = 19) |
26 (23; 28) |
23 (23; 24) |
0.008 |
22 (18; 29) |
26 (25; 27) |
0.024 |
|
Group 4 (n = 16) |
21 (19; 24) |
23 (22; 24) |
0.046 |
31.5 (29; 37) |
27.5 (26; 29) |
0.002 |
Table prepared by the authors using their own data
Note: the data is presented as a value median (Mе) of the lower and upper quartiles Q [ 25–75%].
The analysis of baropodometric parameters in dynamic tests in athletes with PF compared before/after treatment (Fig. 5) revealed a decrease in the CoP velocity in both the frontal and sagittal planes, as well as the statokinesiogram area (p < 0.05). Thus, in athletes from Group 1, the decrease in CoP velocity in the frontal plane was 31%, in athletes from Group 2 — 21%, in patients from Group 3 — 26.6%, and in athletes from Group 4 — 39%. At the same time, the decrease in CoP velocity in the sagittal plane in athletes from Group 1 was 29.4%, in patients from Group 2 — 16.6%, in athletes from Group 3 — 27.7%, and in patients from Group 4 — 37%.
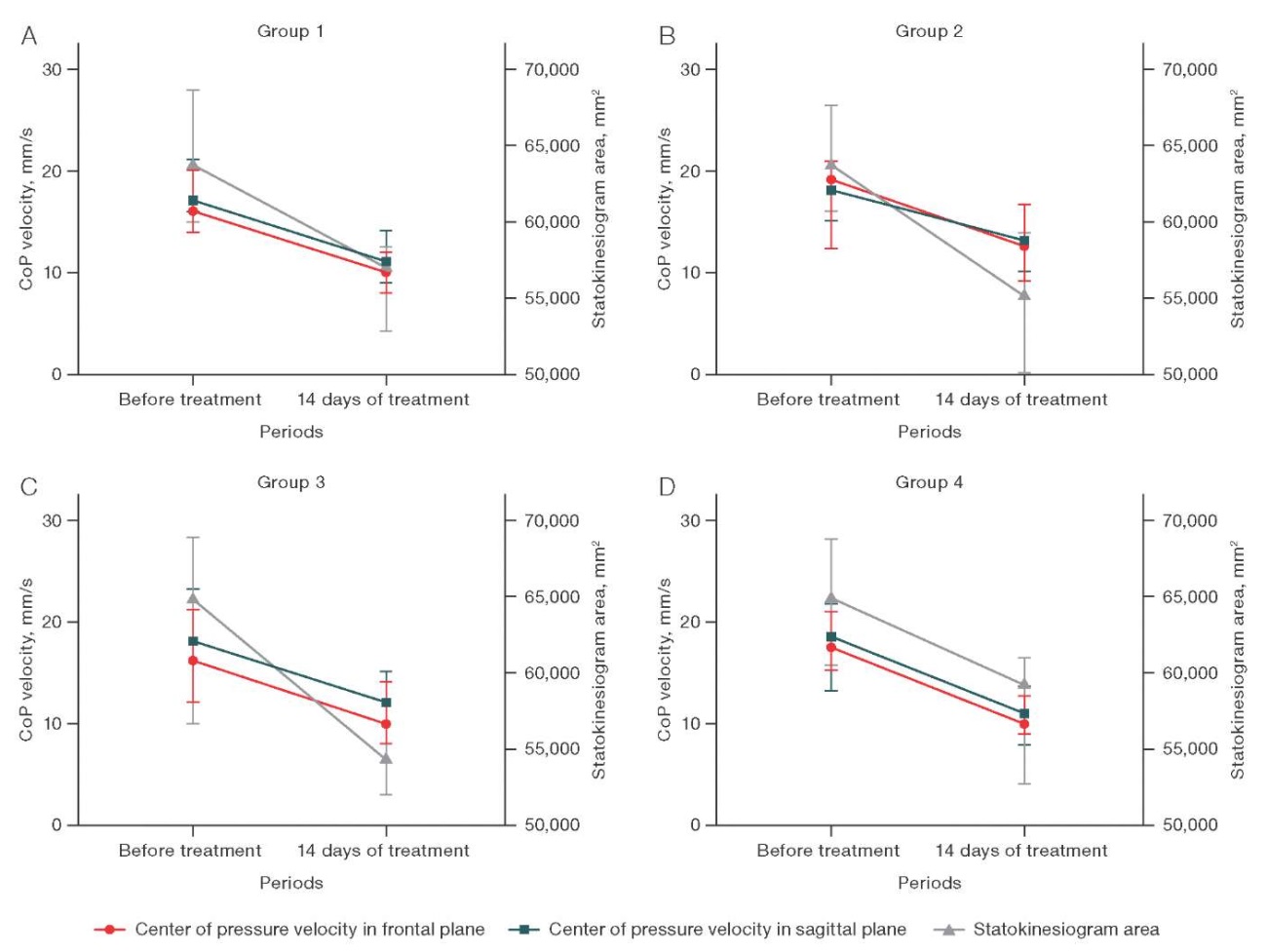
Figure prepared by the authors using their own data
Fig. 5. Changes in baropodometry values in dynamic tests before/after treatment in athletes with PF, depending on the intervention type
There was also a decrease in the statokinesiogram area by 8.7% in athletes from Group 1, in Group 2 — by 12.7%, in Group 3 — by 16.3%, in Group 4 — by 9.2%.
The most pronounced decrease in the CoP velocity was observed in athletes in Group 4 (vibration therapy, myofascial release, and individual orthoses of the feet): by 39% of the CoP velocity in the frontal plane, by 37% of the CoP velocity in the sagittal plane (Fig. 5G). The statokinesiogram area significantly decreased in Group 3 — by 16.3% (Fig. 5B).
Figure 6 shows the results of baropodometry of athletes with PF in follow-up (before treatment/14 days of treatment), reflecting changes in the pressure general vector (PGV) and plantar pressure.
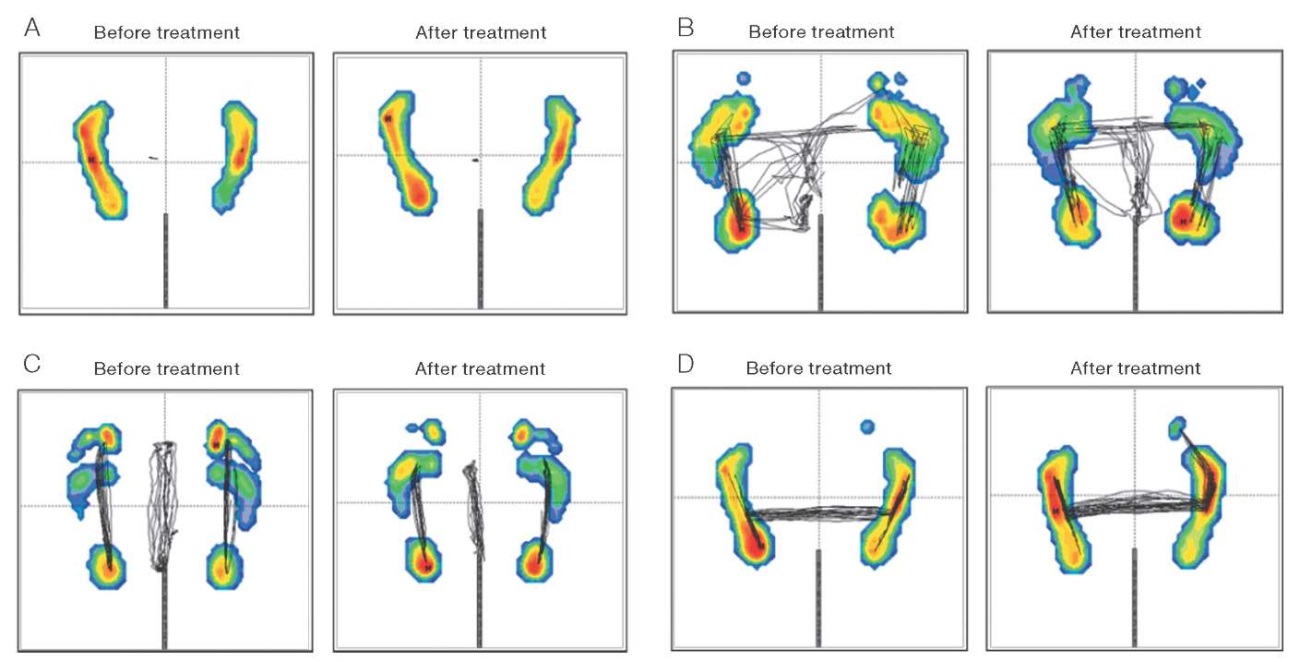
Figure prepared by the authors using their own data
Fig. 6. Baropodometry results of athletes with PF in follow-up
Note: A — in a static test; B — in the jumping dynamic test; C — in the sagittal dynamic test; D — in the frontal dynamic test.
Attention should be drawn to the increase in plantar pressure of the posterior part of the foot in the static test (Fig. 6A), a decrease in the area of PGV distribution and pressure vectors under the feet in the sagittal dynamic test (Fig. 6B), the PGV centralization after curative services in the frontal (Fig. 6C), as well as a decrease in the area of PGV distribution in the jumping dynamic test (Fig. 6D).
The dynamics of changes in the plantar fascia thickness is shown in Fig. 7. In all groups, a statistically significant decrease in the plantar fascia thickness was observed: Group 1 — by 4.8% (p = 0.001), Group 2 — by 5.8% (p = 0.037), Group 3 — by 8.5% (p = 0.008), and Group 4 — by 12.5% (p = 0.012). However, in Groups 1 (ESWT) and 2 (vibration therapy and myofascial release), the change in plantar fascia thickness was less pronounced than in athletes from Groups 3 (individual foot orthoses) and 4 (vibration exposure, myofascial release and individual foot orthoses).
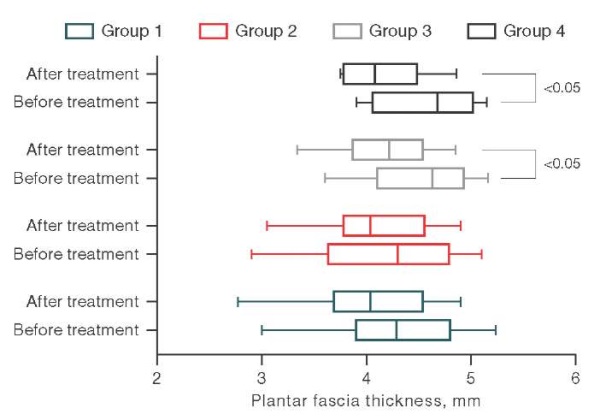
Figure prepared by the authors using their own data
Fig. 7. Plantar fascia thickness before/after treatment in the observation groups
Despite statistically significant changes in the plantar aponeurosis thickness, their pronounced character does not point definitely to clinically significant differences (in particular, in Groups 1 and 2).
DISCUSSION
Our study established a statistically significant decrease in pain by VAS FA in all groups of athletes, which generally indicates the effectiveness of PF corrective measures. Thus, ESWT has been successfully used for PF treatment by some foreign and domestic authors [8][9]. Mendes et al. reported a positive effect of individual orthopedic insoles in terms of pain reduction in patients with PF [10], which was subsequently confirmed by other authors [11][12]. Kırmızı et al. noted the effectiveness of a combined therapy with therapeutic exercises and foot orthoses in reducing pain in patients with PF and flat feet [13].
In our research, pain in the muscles of the posterior shin group decreased statistically significantly in the participants of Group 2, whose therapy used vibration and myofascial release, and Group 3, who used individual orthoses of the feet. This fact can be explained by a significant impact of vibration therapy and individual orthoses of the feet on the activation of the internal and external muscles of the foot, thus contributing to their facilitated inclusion in the act of walking. It was previously suggested that the tenderness and tension of the triceps muscle of the shin, mainly its medial head, may be associated with increased stress on the muscle due to compensation for the insufficient function of the external muscles of the foot, in particular the posterior tibial muscle [14][15]. Moreover, Zhou et al. reported that measures aimed at reducing stiffness and tension in the medial portion of the gastrocnemius muscle could be helpful in reducing the severity of pain in PF patients [15].
The ankle joint dorsiflexion angle increased statistically significantly in Groups 2 (vibration therapy and myofascial release) and 4 (vibration therapy, myofascial release, and individual orthoses of the feet). This seems logical due to vibration and myofascial effects on the muscles of the posterior shin group, which improve their softness and plasticity. In combination with stretching, these measures allowed the volume of ankle joint posterior flexion to be significantly increased, as previously reported by some authors [15–20]. However, Landorf et al. did not find the aforementioned connection [21].
According to the results of baropodometry in PF, normalization of plantar pressure on the affected foot was noted. Thus, in athletes with low plantar pressure in the posterior part of the foot, it increased to normal values, and in athletes with initially high plantar pressure in the posterior part of the foot, on the contrary, decreased. The redistribution of pressure in the posterior part of the foot was also accompanied by normalization of plantar pressure in the anterior part of both the affected foot and the intact (contralateral) foot, in which plantar pressure had previously been compensationally impaired. In addition to the normalization of plantar pressure, all athletes with PF showed an improvement in both general postural stability and local stability during corrective measures, which were assessed based on the results of dynamic tests. At the same time, in Groups 2 (vibration therapy and myofascial release) and 4 (vibration therapy, myofascial release, and individual orthoses of the feet), a greater decrease in the statokinesiogram area in the jumping test was observed, which may indicate the influence of vibration therapy on the overall postural balance by influencing the proprioceptive apparatus. This fact is particularly interesting concerning the possibility of important effects of the pathobiomechanics of the overlying parts of the organs of support and movement (pelvis) on the underlying ones (feet). A similar effect was previously reported by some authors [22–24].
The plantar aponeurosis thickness tended to decrease in all the studied groups, which indicates a decrease in the fascia edema severity. This, in turn, may reflect a decrease in the load on plantar aponeurosis and a decrease in degenerative-inflammatory changes [25][26]. The slight decrease in the plantar fascia thickness can be explained by a short follow-up period (14 days), insufficient to identify clear morphological changes accompanying a clinically significant improvement in athletes with PF. At the same time, Drake et al. noted that changes in the plantar aponeurosis morphology may not always correspond to the patient’s clinical examination data [27].
In our study, the athlete groups were formed by simple randomization, based on the analysis of changes in the observation dynamics. Therefore, it can be concluded that ESWT allows the most effective relief of severe pain in athletes. In addition, individual orthoses of the feet also show significant effectiveness. However, significant risk factors may also influence the choice of the recommended therapeutic agent [28]. Such factors include flat feet, excessive foot pronation, limited ankle joint dorsiflexion, tension and tenderness of the muscles of the posterior shin group, hammer toe deformity [29–32]. Thus, vibration therapy, myofascial release, and individual feet orthoses showed the most pronounced action on correcting/compensating for existing biomechanical risk factors for this disease in athletes. In this connection, it seems advisable to use local treatment methods in the case of an acute process, in order to achieve an anti-inflammatory effect followed by correction of the pathobiomechanics that had triggered the disease. In the case of a sluggish process, correction of impaired biomechanical patterns will not only prevent the development of disease relapses in the future, but also to relieve pain.
Further research should focus on assessing the sustainability of the achieved clinical results in the sports population with a longer follow-up period (12–18 weeks) and the role of therapeutic exercises in preventing possible recurrence of the disease.
CONCLUSION
Our study found that all the therapeutic methods used showed moderate effectiveness in PF treatment in the sports population. The choice of a therapeutic method should be primarily determined by the pain syndrome severity, as well as the foot structural and functional features, identified during a biomechanical examination on a baropodometric platform.
In athletes, the use of a differentiated approach based on a combined therapy aimed at correcting all existing risk factors seems justified. If necessary, ESWT is highly effective for relieving an acute pain syndrome. For achieving good therapeutic effects in the presence of foot deformities, it is advisable to use individual feet orthoses. In the case of limited ankle joint dorsiflexion and muscle tension of the posterior shin group, vibration action in combination with MFR of the muscles of the posterior shin group proves highly effective.
Treatment of athletes with PF is a challenging and lengthy process that does not always result in the resumption of full-fledged sports activities. The use of a combined and algorithmized personalized therapeutic strategy, accounting for significant risk factors for the disease in the sports population, can significantly reduce the duration of rehabilitation treatment for athletes with this pathology, as well as reduce the rate of disease recurrence.
1. Ponomarenko GN, Hajduk AA. The use of individual foot orthoses Formthotics in clinical practice. Guidelines. St. Petersburg; 2015 (In Russ.).
References
1. Trojian T, Tucker AK. Plantar Fasciitis. Am Fam Physician. 2019;99(12):744–50. PMID: 31194492
2. Atzmon R, Eilig D, Dubin J, Vidra M, Marom O, Tavdi A, et al. Comparison of Platelet-Rich Plasma Treatment and Partial Plantar Fasciotomy Surgery in Patients with Chronic Plantar Fasciitis: A Randomized, Prospective Study. J Clin Med. 2022;11(23):6986. https://doi.org/10.3390/jcm11236986
3. Coppola M, Sgadari A, Marasco D, Danti C, Vitale G, Smeraglia F, Balato G, Bernasconi A. Treatment Approaches for Plantar Fasciopathy in Elite Athletes: A Scoping Review of the Literature. Orthop J Sports Med. 2022;10(11):23259671221136496. https://doi.org/10.1177/23259671221136496
4. Wang B, Wang XL, Ma YT, Wu W, Zheng YJ. Evaluation of the efficacy of trigger points combined with extracorporeal shock waves in the treatment of plantar fasciitis: heel temperature and plantar pressure. BMC Musculoskelet Disord. 2024 Mar 2;25(1):191. https://doi.org/10.1186/s12891-024-07296-2 Erratum in: BMC Musculoskelet Disord. 2024;25(1):546. https://doi.org/10.1186/s12891-024-07643-3
5. Pazhooman H, Alamri MS, Pomeroy RL, Cobb SC. Foot kinematics in runners with plantar heel pain during running gait. Gait Posture. 2023;104:15-21. https://doi.org/10.1016/j.gaitpost.2023.05.019
6. Kovaleva MA., Mogelnitskiy AS., Belyaev AF. Validation of Russian-language version of Visual Analog Scale Foot and Ankle (VAS FA). Russian Osteopathic Journal. 2023;(3):34–45 (In Russ.). https://doi.org/10.32885/2220-0975-2023-3-34-45
7. Karmazin VV, Slivin AV, Parastaev SA. Plantar pressure distribution features in athletes with plantar fasciitis. Extreme Medicine. 2024;26(2):87–93 (In Russ.). https://doi.org/10.47183/mes.2024.036
8. Belonogov VN, Kireev SI, Kireev SN, Semenov NS. Application of shock wave therapy in the complex treatment of plantar fasciitis. Saratov Scientific Medical Journal. 2019;15(4):858–61 (In Russ.). EDN: LOOVML
9. Vikhlyantsev VA, Kobelev MV, Shapovalova EM. The mechanism of clinical effectiveness of the radial shock wave method in the treatment of plantar fasciitis. Medical Science and Education of the Urals. 2020;21(2):84–6 (In Russ.). https://doi.org/10.36361/1814-8999-2020-21-2-84-86
10. Mendes AAMT, Silva HJA, Costa ARA, Pinheiro YT, Lins CAA, de Souza MC. Main types of insoles described in the literature and their applicability for musculoskeletal disorders of the lower limbs: A systematic review of clinical studies. J Bodyw Mov Ther. 2020;24(4):29–36. https://doi.org/10.1016/j.jbmt.2020.06.001
11. Schuitema D, Greve C, Postema K, Dekker R, Hijmans JM. Effectiveness of Mechanical Treatment for Plantar Fasciitis: A Systematic Review. J Sport Rehabil. 2019;29(5):657–74. https://doi.org/10.1123/jsr.2019-0036
12. Lewis RD, Wright P, McCarthy LH. Orthotics Compared to Conventional Therapy and Other Non-Surgical Treatments for Plantar Fasciitis. J Okla State Med Assoc. 2015;108(12):596–8.
13. Kirmizi M, Sengul YS, Akcali O, Angin S. Effects of foot exercises and customized arch support insoles on foot posture, plantar force distribution, and balance in people with flexible flatfoot: A randomized controlled trial. Gait Posture. 2024;113:106–14. https://doi.org/10.1016/j.gaitpost.2024.05.030
14. Dayton P. Anatomic, Vascular, and Mechanical Overview of the Achilles Tendon. Clin Podiatr Med Surg. 2017;34(2):107–13. https://doi.org/10.1016/j.cpm.2016.10.002
15. Zhou JP, Yu JF, Feng YN, Liu CL, Su P, Shen SH, Zhang ZJ. Modulation in the elastic properties of gastrocnemius muscle heads in individuals with plantar fasciitis and its relationship with pain. Sci Rep. 2020;10(1):2770. https://doi.org/10.1038/s41598-020-59715-8
16. Cheung JT, Zhang M, An KN. Effect of Achilles tendon loading on plantar fascia tension in the standing foot. Clin Biomech (Bristol). 2006;21(2):194–203. https://doi.org/10.1016/j.clinbiomech.2005.09.016
17. Lee SH, Suh DH, Kim HJ, Jang WY, Park YH, Sung HJ, Choi GW. Association of Ankle Dorsiflexion With Plantar Fasciitis. J Foot Ankle Surg. 2021;60(4):733–7. https://doi.org/10.1053/j.jfas.2021.02.004
18. Nakale NT, Strydom A, Saragas NP, Ferrao PNF. Association Between Plantar Fasciitis and Isolated Gastrocnemius Tightness. Foot Ankle Int. 2018;39(3):271–7. https://doi.org/10.1177/1071100717744175
19. Sullivan J, Burns J, Adams R, Pappas E, Crosbie J. Musculoskeletal and activity-related factors associated with plantar heel pain. Foot Ankle Int. 2015;36(1):37–45. https://doi.org/10.1177/1071100714551021
20. Bolívar YA, Munuera PV, Padillo JP. Relationship between tightness of the posterior muscles of the lower limb and plantar fasciitis. Foot Ankle Int. 2013;34(1):42–8. https://doi.org/10.1177/1071100712459173
21. Landorf KB, Kaminski MR, Munteanu SE, Zammit GV, Menz HB. Clinical measures of foot posture and ankle joint dorsiflexion do not differ in adults with and without plantar heel pain. Sci Rep. 2021;11(1):6451. https://doi.org/10.1038/s41598-021-85520-y
22. Lee JH, Park JH, Jang WY. The effects of hip strengthening exercises in a patient with plantar fasciitis: A case report. Medicine (Baltimore). 2019;98(26):e16258. https://doi.org/10.1097/MD.0000000000016258
23. Lewis CL, Ferris DP. Walking with increased ankle pushoff decreases hip muscle moments. J Biomech. 2008 Jul 19;41(10):2082–9. https://doi.org/10.1016/j.jbiomech.2008.05.013
24. Mueller MJ, Sinacore DR, Hoogstrate S, Daly L. Hip and ankle walking strategies: effect on peak plantar pressures and implications for neuropathic ulceration. Arch Phys Med Rehabil. 1994 Nov;75(11):1196–200. https://doi.org/10.1016/0003-9993(94)90004-3
25. Chimutengwende-Gordon M, O’Donnell P, Singh D. Magnetic resonance imaging in plantar heel pain. Foot Ankle Int. 2010;31(10):865–70. https://doi.org/10.3113/FAI.2010.0865
26. Bicer M, Hocaoglu E, Aksoy S, İnci E, Aktaş İ. Assessment of the Efficacy of Extracorporeal Shockwave Therapy for Plantar Fasciitis with Magnetic Resonance Imaging Findings. J Am Podiatr Med Assoc. 2018;108(2):100–5. https://doi.org/10.7547/15-106
27. Drake C, Whittaker GA, Kaminski MR, Chen J, Keenan AM, Rathleff MS, Robinson P, Landorf KB. Medical imaging for plantar heel pain: a systematic review and meta-analysis. J Foot Ankle Res. 2022;15(1):4. https://doi.org/10.1186/s13047-021-00507-2
28. Tan VAK, Tan CC, Yeo NEM, Zhang M, Mehta KV, Tian RHH, Tan B. Consensus statements and guideline for the diagnosis and management of plantar fasciitis in Singapore. Ann Acad Med Singap. 2024;53(2):101–12. https://doi.org/10.47102/annals-acadmedsg.2023211
29. Martinelli N, Bianchi A, Martinkevich P, Sartorelli E, Romeo G, Bonifacini C, Malerba F. Return to sport activities after subtalar arthroereisis for correction of pediatric flexible flatfoot. J Pediatr Orthop B. 2018;27(1):82–7. https://doi.org/10.1097/BPB.0000000000000449
30. Pohl MB, Hamill J, Davis IS. Biomechanical and anatomic factors associated with a history of plantar fasciitis in female runners. Clin J Sport Med. 2009;19(5):372–6. https://doi.org/10.1097/JSM.0b013e3181b8c270
31. Bencke J, Christiansen D, Jensen K, Okholm A, Sonne-Holm S, Bandholm T. Measuring medial longitudinal arch deformation during gait. A reliability study. Gait Posture. 2012;35(3):400–4. https://doi.org/10.1016/j.gaitpost.2011.10.360
32. Knapik DM, LaTulip S, Salata MJ, Voos JE, Liu RW. Impact of Routine Gastrocnemius Stretching on Ankle Dorsiflexion Flexibility and Injury Rates in High School Basketball Athletes. Orthop J Sports Med. 2019;7(4):2325967119836774. https://doi.org/10.1177/2325967119836774
About the Authors
A. V. SlivinRussian Federation
Anton V. Slivin
Moscow
V. V. Karmazin
Russian Federation
Valerii V. Karmazin
Moscow
K. A. Shlykov
Russian Federation
Kirill A. Shlykov
Moscow
S. A. Parastaev
Russian Federation
Sergey A. Parastaev
Moscow
Supplementary files
Review
For citations:
Slivin A.V., Karmazin V.V., Shlykov K.A., Parastaev S.A. Effectiveness of conservative methods for plantar fasciitis treatment in athletes. Extreme Medicine. 2025;27(1):115-123. https://doi.org/10.47183/mes.2025-270

















