Scroll to:
Role of fibrinolytic system changes in the development of post-stroke cognitive impairments
https://doi.org/10.47183/mes.2025-293
Abstract
Introduction. Post-stroke cognitive impairment (PSCI) is an important medical and social problem, with its prevalence reaching the level of 74%.
Objective. To study the relationship between integral parameters characterizing the processes of coagulation and fibrinolysis, determined using dynamic thrombophotometry, and PSCI formation with the purpose of assessing the possibility of predicting PSCI and adverse disease outcomes.
Materials and methods. The study included 35 patients who had suffered an ischemic stroke within 24 hours of the onset of the disease: 20 (57.1%) women and 15 (42.9%) men; the median age was 66.5 [62.3–73.3] years. The comparison group included 45 conditionally healthy volunteers. Assessment of the state of the hemostasis system was carried out upon admission to the hospital, on days 6–8 and 13–15. Integral indicators evaluating the coagulation, fibrinolysis, and hemostasis systems in general were studied using the Fibrinodynamics method. Cognitive functions were assessed on days 10–14 according to the Montreal Cognitive Assessment (MoCA) scale. The functional outcome of the disease was determined by the Modified Rankin Scale (mRS) on day 28. The SPSS 27.0 software (IBM, USA) was used for statistical analysis. Associations between continuous data were evaluated using the Spearman correlation coefficient, one-dimensional and multidimensional linear regression models. The difference at the level of p < 0.05 was considered statistically significant.
Results. An inverse correlation was found between the average brightness of the clot during the integral modeling of hemostasis processes at admission and the level of cognitive dysfunction on the MoCA scale (rs = –0.409; p = 0.02); higher initial HB values were associated with severe post-stroke cognitive impairment. Conversely, a direct relationship between the initial fibrinolysis of the resulting clot (FB) and cognitive impairment on the MoCA scale (r = 0.512, p = 0.003) was found; higher values of FB corresponded to a higher score on the MoCA scale and a higher level of cognitive functions.
Conclusions. Predictive multidimensional linear regression models that included age and baseline stroke severity found that an increase in baseline HB by every 11.5 arbitrary units or a decrease in baseline FB by 9.8 arbitrary units corresponded to a minus 1 point deterioration in the cognitive status when assessed by MoCA. Patients with higher baseline values of FB had more favorable functional outcomes of the disease according to (mRS). The use of dynamic thrombophotometry and its extended version makes it possible to comprehensively assess changes in the hemostasis system of patients with ischemic stroke. Higher HB values and lower FB values make it possible to predict an unfavorable outcome of the disease and more severe PSCI in the early stages, while the hypoactivation of the fibrinolytic system is associated with a greater severity of PSCI and a less favorable functional outcome.
Keywords
For citations:
Koltsov I.A., Shchukin I.A., Fidler M.S., Karpova N.S., Brusov O.S., Shilov Yu.E., Kovalenko E.A., Boyko A.N. Role of fibrinolytic system changes in the development of post-stroke cognitive impairments. Extreme Medicine. 2025;27(2):169-175. https://doi.org/10.47183/mes.2025-293
INTRODUCTION
Stroke is the leading cause of disability worldwide [1]. The modern development of reperfusion technologies in the treatment of ischemic stroke has significantly improved the outcomes of the disease, at the same time, post-stroke cognitive impairment (PSCI) and especially post-stroke dementia (PSD) are still significant conditions that significantly worsen the quality of life of both patients and their relatives [2]. The PSCI prevalence, according to various sources, ranges 4.4–73% [3]. It should be noted that PSCI is an unfavorable outcome of not only ischemic, but also hemorrhagic stroke [4]. As a rule, the development of a persistent symptom complex peaks in the early recovery period, i.e. 3–6 months after a stroke. In addition to the characteristic disorders of higher cortical functions (aphasic disorders, memory disorders, agnosia, and apraxia) directly associated with damage to certain areas of the brain, patients with PSCI develop symptoms typical of vascular cognitive impairment (CI): impaired attention and regulatory functions [3].
Acute cerebral ischemia is a complex cascade consisting of many pathophysiological links, including prothrombotic and proinflammatory activation at both systemic and local levels. On the one hand, thrombosis of large and small cerebral vessels leads to varying degrees of ischemic damage to brain matter, on the other hand, in parallel with prothrombotic processes, excessive release of proinflammatory cytokines and leukocyte infiltration of ischemic brain areas occur [5]. The relationship between thrombosis and inflammation is commonly referred to as thromboinflammation, and, according to some researchers, is one of the causes of persistent post-stroke disorders, including PSCI [6][7].
Dynamic thrombophotometry is a new method for assessing the state of the hemostasis system, which makes it possible to simulate and register in vitro processes of fibrin clot induced by tissue growth factor under conditions close to physiological conditions. Of particular interest is the modification of the method with the possibility of simultaneous modeling of the processes of fibrin clot growth and lysis, followed by the calculation of the values of a number of integral parameters, “Fibrinodynamics” (FD) [8]. This method allows us to evaluate not only the activation of coagulation and fibrinolysis systems, but also the shift in the balance between them towards thrombosis or hypocoagulation. In addition, this method allows us to determine the indirect contribution of additional factors, such as inflammation and endothelial dysfunction, to the overall balance of the hemostatic system within the framework of the thromboinflammation-immunothrombosis concept [9].
As part of the previous stage of our research, we studied the state of the coagulation link of hemostasis in patients with ischemic stroke (IS) using dynamic thrombophotometry. It was noted that the increase in the optical density of the fibrin clot and its high values can be considered as a possible prognostically significant biomarker of the early development of PSCI [10]. Currently, the study of promising areas for the use of dynamic thrombophotometry, in particular, its modification of FD in predicting the early manifestations of PSCI, is continuing.
The aim of the study was to study the relationship between the integral parameters characterizing the processes of coagulation and fibrinolysis, calculated using dynamic thrombophotometry, and the PSCI development to assess the possibility of predicting PSCI and unfavorable disease outcomes.
MATERIALS AND METHODS
A non-interventional study of the integral parameters of coagulation and fibrinolysis systems and hemostasis in general was conducted at the clinical facilities of the Department of Neurology, Neurosurgery, and Medical Genetics (Faculty of General Medicine, Pirogov Russian National Research Medical University). The main group consisted of 35 patients who suffered an ischemic stroke within 24 h: 20 (57.1%) women and 15 (42.9%) men. The median age was 66.5 [ 62.3–73.3] years.
As a comparison group, a database of laboratory test results was formed for 45 conditionally healthy volunteers: 20 (44.4%) men and 25 (55.6%) women, with a median age of 31.0 [ 23.5–44.5] years. The comparison group was formed because of the pilot nature of this study, and of the need to compare the results obtained with conditionally physiologically normal values in people from the general population who do not suffer from chronic diseases. The inclusion of volunteer patients in the database was carried out in accordance with the principles of good clinical practice and the signing of informed voluntary consent to take venous blood samples and conduct laboratory tests.
The criteria for inclusion in the main group were: a diagnosis of ischemic stroke confirmed in accordance with the requirements of the Russian ischemic stroke guidelines1, admission to the hospital within 24 h of the onset of the disease, age ≥40 years (for patients aged 40–59 years, the presence of at least one confirmed risk factor for ischemic stroke in the anamnesis), score <10 on the National Institutes of Health Stroke Scale (NIHSS), which is used to assess the neurological status, localization of stroke, differential diagnosis and treatment outcomes, planning thrombolytic therapy and monitoring its effectiveness. The NIHSS, translated in the current Russian ischemic stroke guidelines2, includes a number of parameters reflecting the levels of impairment due to acute cerebrovascular disease: the level of consciousness — the level of wakefulness, eyeballs movements, visual fields examination, determination of the functional state of the facial nerve, assessment of the motor function of the upper extremities, assessment of movements coordination, sensitivity testing, identification of speech disorders, detection of perception disorders — hemi-ignoring or neglect, as well as an approximate prognosis of the disease. The criteria for inclusion in the study were the absence of speech and motor disorders that prevent the objectification of the cognitive status of patients, consent to participate in the study, and the absence of anamnestic signs of pre-stroke disorders.
The criteria for non-inclusion were as follows: admission to the hospital later then 24 h of the onset of the disease, regression of neurological symptoms with a confirmed transient ischemic attack, ischemic stroke of other specified etiology (migrainous, hemodynamic, etc.), the presence of oncological, terminal, somatic or other diseases that cause significant changes in hemostasis (including thrombophilia, hemophilia, Disseminated intravascular coagulation (DIC) syndrome, sepsis, etc.), pregnancy, refusal to participate in research work.
Venous blood samples obtained in accordance with the regulations established by the Russian ischemic stroke guidelines were used to study laboratory parameters3.
Hemostasis parameters were assessed in citrated peripheral venous blood samples in a ratio of 1:10. Two-stage centrifugation was performed to obtain platelet-free plasma (15 min at a relative centrifugal acceleration of 1,500 g and 5 minutes at 10,000 g) using CM-6M centrifuge (ELMI, Latvia) and Microspin 12 centrifuge (Biosan, Latvia). To assess the state of the hemostasis system, the Thrombodynamics T-2 analyser system (Hemacore, Russia) was used. An extended technique was used with simultaneous modeling of coagulation and fibrinolysis processes [8]. Based on the results of the study, the parameters characterizing the functioning of coagulation, fibrinolysis, and hemostasis systems were calculated using the formula:
FB = СВ – НВ, (1)
CB (coagulation brightness, arbitrary units) — the average brightness of a clot when modeling the coagulation process;
HB (hemostasis brightness, arbitrary units) — the average brightness of a clot in the integrated modeling of hemostasis processes;
FB (fibrinolysis brightness, arbitrary units) is a parameter that characterizes the activity of the fibrinolysis process of the growing clot.
In the main group, the hemostasis system was assessed upon admission to the hospital, on days 6–8 and days 13–15. In addition, a standard clinical, instrumental, and laboratory examination was performed at the indicated time intervals, and the severity of neurological deficit was assessed on the NIHSS. The patients’ cognitive functions were assessed on days 10–14 using the Montreal Cognitive Assessment (MoCA) scale [11]. The functional outcome was evaluated on day 28 using a Modified Rankine Scale (mRS), which allows a complex assessment of both post-stroke disability and death [12].
The baseline characteristics of the patients in the main group are presented in the previous part of the work [10]. Arterial hypertension (any stage) was observed in 27 (77.1%) patients, type 2 diabetes mellitus — in 11 (31.4%), atrial fibrillation (any form) — in 9 (25.7%), stenosis of the affected artery over 50% of the lumen — in 14 (40.0%). The NIHSS score upon admission was 5 points [4-8]. The characteristics of the patients, as well as the distribution of ischemic stroke subtypes, were comparable to domestic and foreign literature data.
In the comparison group, the laboratory test was performed once.
The SPSS 27.0 software (IBM, USA) was used for statistical analysis. The final sample size was calculated based on the results of an interim statistical analysis of the data (statistical power of 0.95, α value of 0.05). The data normality was tested using the Shapiro-Wilk test. Extreme data values, if any, were excluded from the calculation. The numerical data in the paper is presented as a median with upper and lower quartiles. The Mann-Whitney test in independent samples and the Wilcoxon test in dependent samples were used to compare variables that did not follow a normal distribution. Associations between continuous data were evaluated using the Spearman correlation coefficient, univariate and multivariate linear regression models.
RESULTS AND DISCUSSION
The results of the study of integral parameters of coagulation and fibrinolysis at different time intervals in patients from the main group were compared with the data of conditionally healthy volunteers; the corresponding parameters are shown in the table. Conclusions about the absence of concomitant hematological diseases causing a significant shift in coagulological indications were drawn based on the absence of deviations in the admission of standard coagulography parameters.
In the main group, upon admission, the values of the integral parameters CB and HB were comparable with the group of conditionally healthy volunteers, which confirmed the similar activity of the coagulation system and the similar functional state of the fibrinolysis system in both groups (Table). At the same time, patients with ischemic stroke showed a tendency to hypofibrinolysis (lower values of the FB parameter) of 18.3 [ 10.0–31.9] versus 25.3 [ 21.7–29.9] arbitrary units upon admission (p = 0.068) when comparing the results of volunteers from the comparison group. This characterized the general prothrombogenic state in ischemic stroke with greater resistance of fibrin clots to the fibrinolysis process. The statistical significance of the differences in these parameters was not achieved due to the presence of several conditionally healthy volunteers with extremely low FB values in the comparison group.
By the end of 1st week, patients with ischemic stroke showed a dramatic statistically significant drop in CB, HB, and FB values to 1.3%, 1.2%, and 1.6% of baseline values, respectively, with a shift towards hypocoagulation relative to the comparison group, which may be due to the initiation of antithrombotic therapy after admission. Overall, the shift in all parameters was possibly due to the following explanation. The method used in this work studies the growth of a fibrin clot from a surface covered with a tissue factor, and therefore active antithrombotic therapy led to a corresponding shift in all parameters. By days 13–15, the main group of patients showed a gradual recovery in the overall activity of the coagulation system, but the values remained lower than in the comparison group due to continued antithrombotic therapy. Taking into account the corresponding bias, the parameters of patients from the main group on days 6–8 and 13–15 were not compared with patients from the comparison group.
In the main group of patients, the study did not reveal any associations between the CB index at admission and cognitive status.
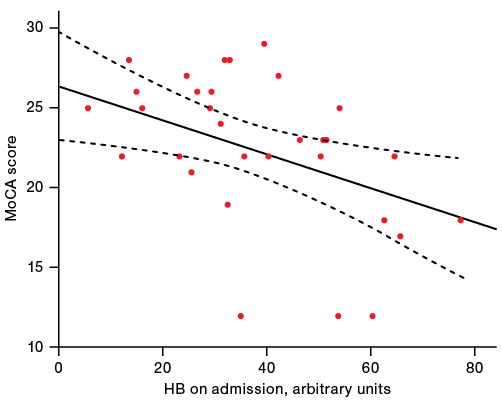
In patients with ischemic stroke, the relationship of HB at admission with a score on the MoCA scale was assessed: higher baseline HB values corresponded to a more pronounced post-stroke cognitive decline (rs = -0.409; p = 0.02); these data are presented in Figure 1. To quantify this association, a simple linear regression model was computed (regression coefficient β = -0.106; 95% CI 0.188-0.024; p = 0.022).
To account for the influence of additional factors (age and initial stroke severity on the NIHSS), a multivariate linear regression model was constructed (regression coefficient β = -0.087; 95% CI from -0.159 to -0.015; p = 0.019). It was found that every 11.5 arbitrary units of increase in the initial HB corresponded to a subsequent deterioration in cognitive status according to MoCA (attention and concentration, control functions, memory, language functions, visual-constructive skills, abstract thinking, counting and orientation) by -1 point. By days 6–8 and 13–15, this association of variables was similar, but did not reach statistical significance.
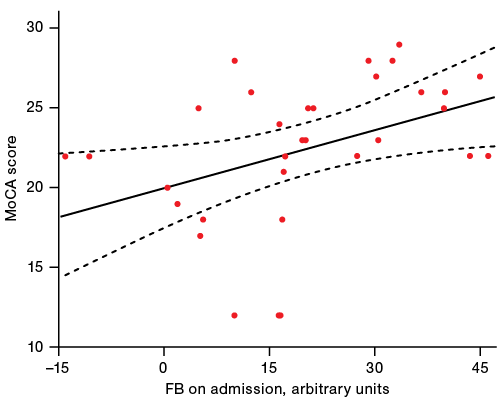
The association of the initial activity of the fibrinolysis process and cognitive function on the MoCA scale was also evaluated. It was revealed that higher values of FB correspond to a higher score on the MoCA scale and, consequently, a higher level of cognitive functions (rs = 0.512; p = 0.003); the corresponding data are presented in Figure 2.
To quantify the predictive significance of this relationship in detail, a simple linear regression model was constructed (regression coefficient β = 0.121; 95% CI 0.018–0.223; p = 0.022).
In order to account the influence of age and the initial severity of focal neurological symptoms on the development of cognitive impairment subsequently, a multivariate model was computed (regression coefficient β = 0.102; 95% CI 0.014–0.190; p = 0.025). It was found that every 9.8 arbitrary units of the initial FB shift towards hypofibrinolysis corresponded to a -1 point deterioration in cognitive status when assessed by MoCA. This relationship persisted by days 6–8 and 13–15 of follow-up, but did not reach statistical significance.
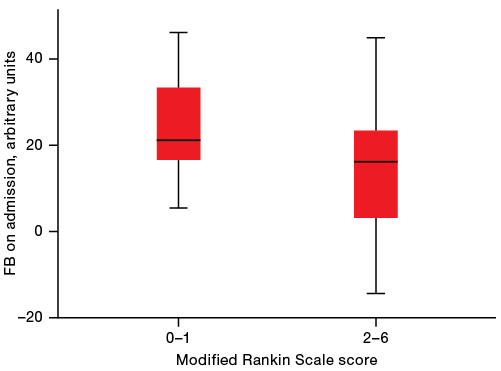
Notably, when comparing participants with mRS scores of 0–1 and participants with mRS scores of 2–6, ischemic stroke patients (n = 17) with excessive FB values, indicative of elevated fibrinolytic system activity, had more favorable functional outcomes at discharge (21.2 [ 16.6–35.0] and 16.2 [ 1.9–27.4] arbitrary units, respectively; p = 0.033) (Fig. 3).
On the first day in patients with ischemic stroke, there were no significant signs of a major shift in the activity of the coagulation and fibrinolytic processes of the hemostasis system beyond the “hematological norm”. At the same time, there was a tendency to lower FB values relative to the comparison group, which may indicate a relative hypofibrinolytic state in acute ischemic stroke [13][14]. It was found that higher values of the patient’s HB on the first day of stroke are potentially associated with a greater severity of cognitive impairment when assessed using the MoCA scale. On the contrary, higher baseline values of the patients’ FB, characteristic of relative hypofibrinolysis, are associated with a smaller cognitive defect later, as well as with a more favorable functional outcome classified using the modified Rankine scale. Comparable results indicating the importance of hypercoagulation conditions in acute vascular diseases are also presented in coronary heart disease [15].
Considering the above, it can be assumed that an important contribution to the development of PSCI is made not only by damage to a certain volume of brain matter as a result of critical ischemia associated with occlusion of the vessel supplying the corresponding zone [16], but also by changes at the level of the microvasculature [17], such as ongoing microthrombosis of small vessels in the hypoperfused region surrounding the infarct core [18][19].
Patients with more active fibrinolysis had more favorable outcomes. The data obtained in this work correlate with the results of the first part of our study, which showed that a higher optical density of a fibrin clot is associated with lower MoCA scores in such patients [10]. It should be noted that recently a number of works have appeared that show the role of fibrin in triggering thromboinflammation processes. In particular, there is evidence that in coronavirus infection, fibrin binds to viral proteins and forms blood clots that activate a systemic inflammatory response that potentiates further thrombotic complications [20].
Table. Dynamics of parameters of the hemostasis system in the main group and the comparison group
|
Parameter |
Main group (n = 35) |
Comparison group (n = 45) |
||
|
On admission |
Days 6–8 |
Days 13–15 |
||
|
CB, arbitrary units |
64.0 [ 42.4–72.8] |
0.8 [ 0.1–7.5]* |
14.9 [ 9.1–22.7]* |
63.3 [ 53.7–73.6] |
|
HB, arbitrary units |
33.9 [ 24.8–51.4] |
0.4 [ 0.1–3.0]* |
8.4 [ 6.3–7.6]* |
37.4 [ 31.0–49.4] |
|
FB, arbitrary units |
18.3 [ 10.0–31.9] |
0.3 [ 0–3.6]* |
5.6 [ 3.4–7.6]* |
25.3 [ 21.7–29.9] |
The table is prepared by the authors using their own data
Note: * — p < 0.001 the level of statistical significance compared to the values at admission (Wilcoxon criterion).
The figure is prepared by the authors using their own data
Fig. 1. Association between the HB (integral assessment of hemostasis system activity) and the MoCA score
The figure is prepared by the authors using their own data
Fig. 2. Association between FB (fibrinolysis integral assessment) and cognitive status evaluated by the MoCA scale
The figure is prepared by the authors using their own data
Fig. 3. Integral assessment of fibrinolysis in different functional outcomes of the disease
CONCLUSION
Post-stroke cognitive impairment, including PSD, is an important medical and social problem. The study of various predictors of the PSCI development in the acute period of stroke is extremely relevant, as this may potentially allow the development of new therapeutic and rehabilitative approaches that may improve the functional outcome in patients with cute cerebrovascular accidents.
A combined laboratory assessment of hypercoagulation and hypofibrinolysis development mechanisms using dynamic thrombophotometry and its extended version of FD allows for a comprehensive measurement of hemostatic shifts in stroke patients and evaluation of systemic and local effects (i.e., thromboinflammation) cumulative contribution to hemostasis activity.
In this research paper, we outlined fibrin clot optical density changes when modeling fibrinolysis and estimating the HB integral parameter. It was found that an increase in the optical density index of a fibrin clot, which characterizes coagulation activity, is associated with a low score on the MoCA scale.
In predictive multivariate linear regression models that included age and baseline stroke severity, it was shown that every 11.5 arbitrary units increase in baseline HB corresponds to a –1 point deterioration in cognitive status when assessed by MoCA. A 9.8% shift in the initial FB values towards hypofibrinolysis was associated with a deterioration in cognitive status and a -1 shift in the MoCA score. The combination of HB and FB parameters made it possible to predict more severe PSCI.
Thus, the study of the hemostasis system using dynamic thrombophotometry and its extended version of FD seems to be extremely relevant and promising in patients with various vascular diseases. This method makes it possible to better predict the probability of unfavorable stroke outcomes. In addition, changes in fibrinolytic activity and the state of the coagulation system are directly related to the activation of systemic inflammation processes, the assessment of which, in conjunction with the study of dynamic thrombophotometry, is a promising but understudied scientific field.
1. Clinical guidelines «Ischemic stroke and transient ischemic attack in adults». Ministry of Health of the Russian Federation; 2021
2. Ibid.
3. Ibid.
References
1. GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Lond Engl. 2018;392(10159):1859–922. https://doi.org/10.1016/S0140-6736(18)32335-3
2. Jokinen H, Melkas S, Ylikoski R, et al. Post-stroke cognitive impairment is common even after successful clinical recovery. Eur J Neurol. 2015;22(9):1288–94. https://doi.org/10.1111/ene.12743
3. Rost NS, Brodtmann A, Pase MP, et al. Post-Stroke Cognitive Impairment and Dementia. Circ Res. 2022;130(8):1252–71. https://doi.org/10.1161/CIRCRESAHA.122.319951
4. Moulin S, Labreuche J, Bombois S, et al. Dementia risk after spontaneous intracerebral haemorrhage: a prospective cohort study. Lancet Neurol. 2016;15(8):820–9. https://doi.org/10.1016/S1474-4422(16)00130-7
5. Steubing RD, Szepanowski F, David C, et al. Platelet depletion does not alter long-term functional outcome after cerebral ischaemia in mice. Brain Behav Immun — Health. 2022;24:100493. https://doi.org/10.1016/j.bbih.2022.100493
6. De Meyer SF, Langhauser F, Haupeltshofer S, Kleinschnitz C, Casas AI. Thromboinflammation in Brain Ischemia: Recent Updates and Future Perspectives. Stroke. 2022;53(5):1487–99. https://doi.org/10.1161/STROKEAHA.122.038733
7. Szepanowski RD, Haupeltshofer S, Vonhof SE, Frank B, Kleinschnitz C, Casas AI. Thromboinflammatory challenges in stroke pathophysiology. Semin Immunopathol. 2023;45(3):389–410. https://doi.org/10.1007/s00281-023-00994-4
8. Karpova NS, Brusov OS, Oleichik IV, Stolyarov SA, Klyushnik TP. Hemostasis System in Patients with Schizophrenia and Schizophrenia Spectrum Disorders. Bull Exp Biol Med. 2024;176(3):390–3. https://doi.org/10.1007/s10517-024-06030-1
9. Koltsov IA, Shchukin IA, Chubykin VI, Fidler M.S. Neuroinflammation And Thromboinflammation In Cerebrovascular Disease And Vascular Cognitive Impairment. Terapiya. 2022;9 (In Russ.). https://doi.org/10.18565/therapy.2022.9.75-81
10. Koltsov IA, Shchukin IA, Kovalenko EA, Karpova NS, Shilov YE, Brusov OS. The relationship between the development of post-stroke cognitive impairment and changes in the coagulation component of hemostasis. S.S. Korsakov Journal of Neurology and Psychiatry. 2024;124(3-2):23–9 (In Russ.). https://doi.org/10.17116/jnevro202412403223
11. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, Cummings JL, Chertkow H. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9. https://doi.org/10.1111/j.1532-5415.2005.53221.x
12. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19(5):604–7. https://doi.org/10.1161/01.str.19.5.604
13. Barakzie A, Jansen AJG, Ten Cate H, de Maat MPM. Coagulation biomarkers for ischemic stroke. Res Pract Thromb Haemost. 2023;7(4):100160. https://doi.org/10.1016/j.rpth.2023.100160
14. de Bruijne EL, Gils A, Rijken DC, de Maat MP, Guimarães AH, Poldermans D, Declerck PJ, Leebeek FW. High thrombin activatable fibrinolysis inhibitor levels are associated with an increased risk of premature peripheral arterial disease. Thromb Res. 2011;127(3):254–8. https://doi.org/10.1016/j.thromres.2010.11.026
15. Reddel CJ, Curnow JL, Voitl J, Rosenov A, Pennings GJ, Morel-Kopp MC, Brieger DB. Detection of hypofibrinolysis in stable coronary artery disease using the overall haemostatic potential assay. Thromb Res. 2013;131(5):457–62. https://doi.org/10.1016/j.thromres.2013.03.015
16. Lee M, Yeo NY, Ahn HJ, Lim JS, Kim Y, Lee SH, Oh MS, Lee BC, Yu KH, Kim C. Prediction of post-stroke cognitive impairment after acute ischemic stroke using machine learning. Alzheimers Res Ther. 2023;15(1):147 (In Russ.). https://doi.org/10.1186/s13195-023-01289-4
17. He Z, Sun J. The role of the neurovascular unit in vascular cognitive impairment: Current evidence and future perspectives. Neurobiol Dis. 2025;204:106772. https://doi.org/10.1016/j.nbd.2024.106772
18. Jacqmarcq C, Picot A, Flon J, Lebrun F, Martinez de Lizarrondo S, Naveau M, Bernay B, Goux D, Rubio M, Malzert-Fréon A, Michel A, Proamer F, Mangin P, Gauberti M, Vivien D, Bonnard T. MRI-based microthrombi detection in stroke with polydopamine iron oxide. Nat Commun. 2024;15(1):5070. https://doi.org/10.1038/s41467-024-49480-x
19. De Silva TM, Faraci FM. Microvascular Dysfunction and Cognitive Impairment. Cell Mol Neurobiol. 2016;36(2):241–58. https://doi.org/10.1007/s10571-015-0308-1
20. Ryu JK, Yan Z, Montano M, et al. Fibrin drives thromboinflammation and neuropathology in COVID-19. Nature. 2024;633(8031). https://doi.org/10.1038/s41586-024-07873-4
About the Authors
I. A. KoltsovRussian Federation
Ivan A. Koltsov, Cand. Sci. (Med.)
Moscow
I. A. Shchukin
Russian Federation
Ivan A. Shchukin, Cand. Sci. (Med.)
Moscow
M. S. Fidler
Russian Federation
Mikhail S. Fidler
Moscow
N. S. Karpova
Russian Federation
Natalia S. Karpova
Moscow
O. S. Brusov
Russian Federation
Oleg S. Brusov, Cand. Sci. (Biol.)
Moscow
Yu. E. Shilov
Russian Federation
Yuri E. Shilov, Cand. Sci. (Biol.)
Moscow
E. A. Kovalenko
Russian Federation
Ekaterina A. Kovalenko, Cand. Sci. (Med.)
Moscow
A. N. Boyko
Russian Federation
Alexey N. Boyko, Dr. Sci. (Med.)
Moscow
Supplementary files
Review
For citations:
Koltsov I.A., Shchukin I.A., Fidler M.S., Karpova N.S., Brusov O.S., Shilov Yu.E., Kovalenko E.A., Boyko A.N. Role of fibrinolytic system changes in the development of post-stroke cognitive impairments. Extreme Medicine. 2025;27(2):169-175. https://doi.org/10.47183/mes.2025-293

















