Scroll to:
Identification of neglect syndrome in cerebral stroke patients using standard tests and eye tracking method
https://doi.org/10.47183/mes.2025-308
Abstract
Introduction. About 30–40% of patients who have suffered from acute cerebrovascular accident (ACVA) experience a syndrome of unilateral spatial neglect. Neuropsychological testing (NT) is a routine diagnostic technique, while the method eye tracking offers prospects for an objective assessment of visual attention.
Objective. Evaluation of the diagnostic capabilities of classical neuropsychological techniques and eye tracking to detect the neglect syndrome in stroke patients.
Materials and methods. The study involved 38 stroke patients (25 men, 13 women; mean age 59.7 ± 12.7 years). The Bells test (BT), Albert’s test (AT), Line bisection test (LBS), the computer version of the Apple test (ApT), and the eye tracking method (a search task for recording visual activity) were used to diagnose the neglect syndrome.
Results. The LBS test data demonstrated the greatest sensitivity in the detection of neglect syndrome. Significant correlations (p < 0.01) were obtained between the results of BT, AT, LBS, and ApT and the results of eye tracker visual search (p = 0.025), indicating the detection of a similar degree of observed deficiency by different methods. The latency of finding stimuli in the left half-field when performing a search task on an eye tracker is significantly higher than in the right side (p < 0.001). Ischemic stroke patients performed AT worse (p = 0.009) than hemorrhagic stroke patients, and they were more mistaken in LBS (p = 0.043). The more pronounced severity of the patients’ neglect, the worse the AT (p = 0.004), LBS (p = 0.05), and Aptego (p = 0.036) were performed. The visual impairment factor had a significant effect in LBS testing (p = 0.02).
Conclusions. The combination of neuropsychological tests and eye tracking provides objective data for the diagnosis of neglect syndrome. The LBS test demonstrated the greatest sensitivity in detecting the neglect syndrome. The results of eye tracking were found to be comparable with those of pencil-and-paper tests, which increases the accuracy of the diagnosis of neglect syndrome. The following factors influencing the performance of diagnostic tests were identified: stroke type, neglect severity, and visual impairment.
Keywords
For citations:
Aizenshtein A.D., Shurupova M.A., Eneeva S.A., Ivanova G.E. Identification of neglect syndrome in cerebral stroke patients using standard tests and eye tracking method. Extreme Medicine. 2025;27(2):161-168. https://doi.org/10.47183/mes.2025-308
INTRODUCTION
About 30–40% of patients who have suffered from acute cerebrovascular accident (ACVA) develop sensory inattention, which refers to the manifestation of visuospatial gnostic disorders [1][2]. In the middle of the last century, ophthalmologist S. Duke Elder coined the term of unilateral spatial agnosia [2][3].
Unilateral spatial neglect is most often defined as the inability to perceive stimuli of various modalities or to respond to these stimuli from the side contralateral to the lesion. In addition, this syndrome includes the absence of voluntary movement of the contralateral side of the body or limb [4], while the physical ability to perform an action remains [5]. A systematic review of neglect syndrome cases after stroke [6] identified this syndrome in 18% of patients with left hemisphere stroke and in 38% with right hemisphere stroke, persisting in 20% of patients in the chronic phase.
It is customary to distinguish different types of neglect based on the disorder modality, the specifics of the lesion of the spatial component of perception and orientation to the stimulus, object or subject of perception. Thus, perceptual, visual, tactile, and auditory ignoring can be distinguished [5]. In addition, the phenomenon of representational and motor disregard, disorder of the voluntary movement of the opposite limb/sides of the body should be mentioned [5].
Depending on the spatial component, personal neglect (ignoring new and familiar stimuli on the body surface), peripersonal neglect (ignoring at arm’s length), and extrapersonal neglect (ignoring stimuli at a distance far from the subject) are distinguished [5]. In determining the ignoring syndrome in the clinical picture of post-stroke disorders, special attention should be paid to the orientation of ignoring. In case of egocentric neglect, the patient ignores all stimuli on the left relative to themselves. In case of allocentric disregard, the patient will ignore the left side of the perceived objects, regardless of their location in space [7].
Due to the variety of ignoring manifestations, the similarity of the disorder pattern with visual disorders, as well as the high frequency of the phenomenon, methods for the diagnosis of neglect are acquiring particular importance. In 2021, the World Federation for Neurorehabilitation issued clinical guidelines outlining the main methods for diagnosing neglect [1].
The most commonly used methods used in neuropsychological practice are aimed at finding and labeling objects. These are so-called pencil-and-paper tests, including Albert’s test, Bells test, Apple test, etc. Pencil-and-paper tests are considered suitable to diagnose and determine neglect due to the possibility of quantifying the performance of tests, as well as their high constructive validity [8].
Line bisection tests are also frequently used, with the most popular option being the Schenkerberg line bisection test (LBS). Using this test, the researcher is capable of estimating the percentage of displacement of the subjective visual midline. In clinical practice, tests for spontaneous drawing, writing, copying, and reproducing objects are also applied. These tests determine the level of disorder of visuospatial and representative representations. In addition, they may reflect the patient’s ignoring of the left side of the presented stimuli [9][10]. Despite the variety of pencil-and-paper tests, they are less sensitive in the assessment of attention and perception in the extrapersonal space, failing to solve the problem of differentiating the motor or visual type of ignoring [2].
In the diagnostics of ignoring syndrome, a strategy for scanning the patient’s space should be selected. From this point of view, the most informative research methods are oculography and eye tracking. The latter approach can be used to track the movement of the subject’s gaze, the number of gaze fixations, the duration of fixations, etc., thus providing objective quantitative data for analysis. A number of studies indicated the high diagnostic significance of the method, as well as its greater sensitivity to the manifestations of the syndrome in comparison with cancellation tests [11]. The important advantage of the eye-tracking technique consists in the absence of the need to involve a motor component in the testing process, which makes it possible to differentiate between motor and visual ignoring, visual-motor delay. However, although the eye-tracking method shows high potential in solving various diagnostic tasks, it does not provide the opportunity to assess attention and perception in the peripersonal space and is ineffective in patients with visual impairment [2].
The World Federation for Neurorehabilitation has outlined an approach to the diagnosis of neglect, which consists in using more than two different types of diagnostic tests. Nevertheless, the current literature lacks studies aimed at assessing the diagnostic significance of an integrated approach based on the use of cancellation tests and hardware methods [1].
In this research, we set out to evaluate the diagnostic capabilities of classical neuropsychological tests and eye tracking to detect the neglect syndrome in stroke patients.
MATERIALS AND METHODS
Study participants
The conducted research was an observational, cross-sectional, and prospective study aimed at an in-depth diagnostic examination of neglect syndrome signs in patients undergoing rehabilitation at the Federal Center of Brain Research and Neurotechnologies.
Initially, the sample included 49 patients who had suffered a cerebral stroke. The inclusion criteria were a first history of stroke, less than 12 months after the stroke, visual acuity from –3 to +2D, the presence or suspicion of neglect syndrome (by neuropsychologist conclusion), understanding of instructions, ≥3 points on the rehabilitation routing scale (RRS). The exclusion criteria were repeated stroke, more than 12 months after stroke, aphasia, multiple hospitalizations for rehabilitation, right-sided hemianopsia, and other neurological lesions.
After excluding patients according to the criteria, the final sample consisted of 38 patients (25 males; 13 females; mean age 59.7 ± 12.7 years). The characteristics of the sample are presented in Table 1. The neglect syndrome and its severity were diagnosed by a neuropsychologist during a classical neuropsychological examination. According to the neuropsychologist conclusion regarding the patients without a neglect syndrome (in six out of 38 patients, the syndrome severity had not been detected), an assumption was made about its presence or the presence of other visuospatial disorders. Based on the calculated proportion of patients with the diagnosed neglect syndrome, all the examined patients were divided into two groups: those with a neglect syndrome H+ (32 people) and those without a neglect syndrome H– (six people). Decreased vision was determined according to objective ophthalmological examination data and/or subjective complaints of the patients.
Table 1. Integral characteristics of the final sample of patients
|
Sign |
Sign gradation |
Patient number, N |
|
Stroke type |
ischemic hemorrhagic |
28 (74%) 10 (28%) |
|
Stroke focus localization |
RMCA RH VBS |
23 (61%) 13 (34%) 2 (5%) |
|
Neglect syndrome |
present absent |
32 (84%) 6 (16%) |
|
Neglect severity |
Unknown mild moderate moderate-severe severe |
6 (16%) 8 (21%) 15 (39%) 5 (13%) 4 (11%) |
|
Decreased visual acuity |
present absent |
18 (47%) 20 (3%) |
Table prepared by the authors using their own data
Note: RMCA — right middle cerebral artery; RH — right hemisphere; VBS — vertebrobasilar system.
RESEARCH DESIGN
A number of conventional neuropsychological tests were used to diagnose neglect syndrome, as well as a search task using the eye tracking method. For performing pencil-and-paper tests (Albert’s test, Balls test, Line Bisection test), pencil and paper were used, while the patient was seated at a table, and the middle line of his body correlated with the middle line of the sheet.
Albert’s test (AT) — the test of crossing out short lines, the maximum score is 41 [12]. The neglect syndrome is diagnosed with more than 70% of the left missed lines from the total number of missed lines.
Bells test (BT) — the maximum score in this test is 35; less than 29 points indicate the presence of neglect syndrome [13]. The sum of the crossed-out points in the left, center, and right parts of the form is estimated using a template.
Line bisection test (LBS) — the test divides straight lines in half; the author of the test recommended considering dividing only the left lines [14].
The test results were calculated using the following formula:
Percentage of deviation = (patient’s mark is the mark of the true center) / (mark of the true center) × 100%.
The percentage of deviation from the true “0” on the left side will have a negative sign, on the right — a positive sign. If the value averaged over all left lines is >7%, the neglect syndrome is diagnosed (according to the norm established in the domestic neurotypical sample: N = 38 people, average age 49.8 ± 12.1 years; the calculated threshold for determining neglect is 7%). The higher the percentage, the more pronounced the neglect severity.
Apple test (ApT) — the test of crossing out closed (whole) circles [15]. In this study, a computerized version was used, containing 90 circles, 30 of each type (closed, unclosed on the left, unclosed on the right) The test allows the researcher to identify the neglect syndrome and determine its type: allocentric (allo) or egocentric (ego). The neglect syndrome is confirmed in the presence of three or more common errors (according to W.H. Jang, with modifications) [16]. To determine the egocentric type of neglect (ignoring one side of the space relative to one’s own body), the difference between the right and left half of the screen in uncrossed whole circles was taken into account, which should be at least one unit. For an allocentric neglect (ignoring one side of objects, regardless of their location in space relative to the body), the difference between crossed-out non-closed circles on the left and on the right was also taken into account, as well as at least one unit. During the test, the patient’s head was fixed in the frontal-chin support, which was performed using a computer mouse.
The visual search task was performed by a C-EyePro device, AssisTechSp. (z.o.o., Poland) [17] using the eye tracking technology. Eye tracking is a method for video recording of eye movements using video in infrared light to detect pupil position; the method determines patterns of gaze fixation when viewing a visual scene, as well as calculate quantitative characteristics, including the frequency of fixations and saccades, duration of fixations, amplitude of saccades, etc. The task was to detect a target object (brightness; realistic objects of various shapes, such as a soccer ball, a light bulb, a felt-tip pen, etc.) located in the left or right half-field of vision among a variety of distractors; each of the six samples began with a fixation stimulus from the center. The latency of finding the target object in each sample was recorded. If the patient did not find the object in more than 30 seconds, this sample was not counted.
Statistical data analysis was performed using the JASP 0.18.3 package (JASP Team, the Netherlands). Taking into account the small sample size, nonparametric statistical methods were used for data analysis. The Mann–Whitney nonparametric criterion was used for comparative intergroup analysis, the Spearman criterion for correlation analysis, and the Kruskal–Wallis criterion for analyzing the influence of clinical factors. Differences with a statistical significance level of less than 0.05 were considered significant.
RESULTS
Neglect syndrome diagnostics by neuropsychological tests
The study determined the proportion of patients who showed the signs of neglect syndrome according to the thresholds of each neuropsychological test; the corresponding data are shown in Fig. 1. Thus, 35 (93%) patients were diagnosed with neglect syndrome based on the LBS test results, compared to the AT technique — 15 (40%) patients, the Bells test method — 25 (67%) patients, the Apple test ego (ApTego) — 27 (71%) patients, and Apple test allo (ApTallo) — 22 (57%) patients.
According to the calculated proportions, groups of patients with and without neglect syndrome were formed, and intergroup comparisons of the results of each neuropsychological test were conducted (Table 2, Fig. 2), with the exception of LBS, due to the small number of patients without neglect.
When analyzing the differences between the two groups relative to the thresholds in patients with (H+), a statistically significant deterioration in test performance was found in the score: AT by 32%, BT by 56%, ApTego by 75%, ApTallo by 8.3%. At the same time, patients performed LBS test tasks less accurately by 33.5% compared to the results of patients in the (H–) group.
Intergroup comparisons show that patients with neglect syndrome perform statistically significantly worse on all tests (score lower in AT and BT, crossing out fewer objects; score higher in ApT, leaving more objects uncrossed) than patients without neglect.
Diagnosis of visual attention by eye tracking
To identify differences in the perception of stimuli in the left and right half-fields in all patients, an analysis of the latency of finding stimuli, averaged over all samples for each side, was performed. The results showed that patients found stimuli in the right half-field much faster, requiring an average of 1.43 s compared to 15.37 s to find a stimulus in the left half-field (p < 0.001).
Comparison of the results of neuropsychological tests and eye tracking diagnostics
To identify associations between the results obtained using neuropsychological tests and the average latency of finding the target stimulus in the search task on the tracker, Spearman’s rank correlation (rs) analysis was performed; the corresponding data are presented in Table 3.
Significant correlations were found between the results obtained on the tracker, BT, and AT, Thus, the worse patients coped with these tests, the slower they managed to find objects on the left on the eye tracker. Interestingly, the results of performing ApT with the detection of an allocentric defect have a weak correlation with the tendency to reliability only with the results of eye tracker diagnostics (rs = 0.370; p = 0.090).
Influence of clinical factors on the results of neuropsychological tests and eye tracking
It was found that patients with ischemic stroke performed worse than those with hemorrhagic stroke AT (H(1.37) = 6.82, p = 0.009), and made more mistakes when performing LBS (H(1.27) = 4.61, p = 0.043); in other tests, the influence of the factor was not detected.
The more pronounced the severity of the defect in the patient, the worse the AT (H(4.31) = 7.27, p = 0.004), LBS (H(4.27) = 2.79, p = 0.05), ApTego- (H(4.27) = 3.09, p = 0.036) were performed. In BT, a similar dynamics was observed, although insignificant (H(4.31) = 4.25, p = 0.333); the corresponding data are shown in Fig. 3.
The visual impairment factor had a significant effect when performing LBS tasks (H(1.27) = 6.11, p = 0.02), at the level of statistical significance trends when performing AT (H(1.37) = 3.86, p = 0.057) and the eye tracker search task (H(1.28) = 3.33, p = 0.07). In other words, patients with a decreased vision performed worse on these tests.
The time elapsed after the stroke had no effect on the results of any tests.
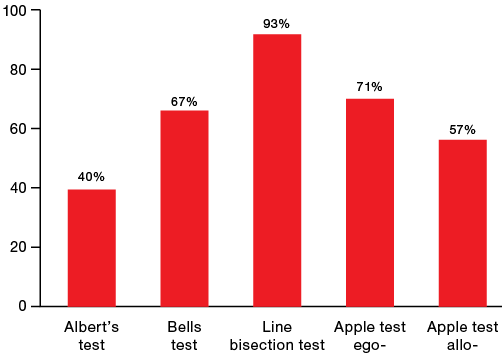
Figure prepared by the authors
Fig. 1. Proportion of patients with diagnosed neglect syndrome according to the threshold value of each neuropsychological test
Table 2. Intergroup comparisons of patients without (H-) and patients with (H+) neglect on each of the neuropsychological tests
|
Parameter |
Albert’s test, scores |
Bells test, scores |
Line bisection test, % |
Apple test, scores |
||||||
|
ego- |
allo- |
|||||||||
|
Н- (n = 23) |
Н+ (n = 15) |
Н- (n = 13) |
Н+ (n = 25) |
Н- (n = 3) |
Н+ (n = 35) |
Н- (n = 11) |
Н+ (n = 27) |
Н- (n = 16) |
Н+ (n = 22) |
|
|
Me [Q1; Q3] |
41 [ 41; 41] |
28 [ 21; 33] |
31 [ 30; 32] |
11.5 [ 9; 22] |
–9 [ –11; –7] |
42.5 [ 20; 55] |
0 [ 0; 0] |
7.5 [ 3; 20] |
0 [ 0; 0] |
2.5 [ 1; 7] |
|
p Mann-Whitney |
<0.001 |
<0.001 |
– |
<0.001 |
<0.001 |
|||||
Table prepared by the authors using their own data
Note: the data is presented as the median Me [Q1; Q3]; “–” could not be performed due to the small number of patients without neglect.
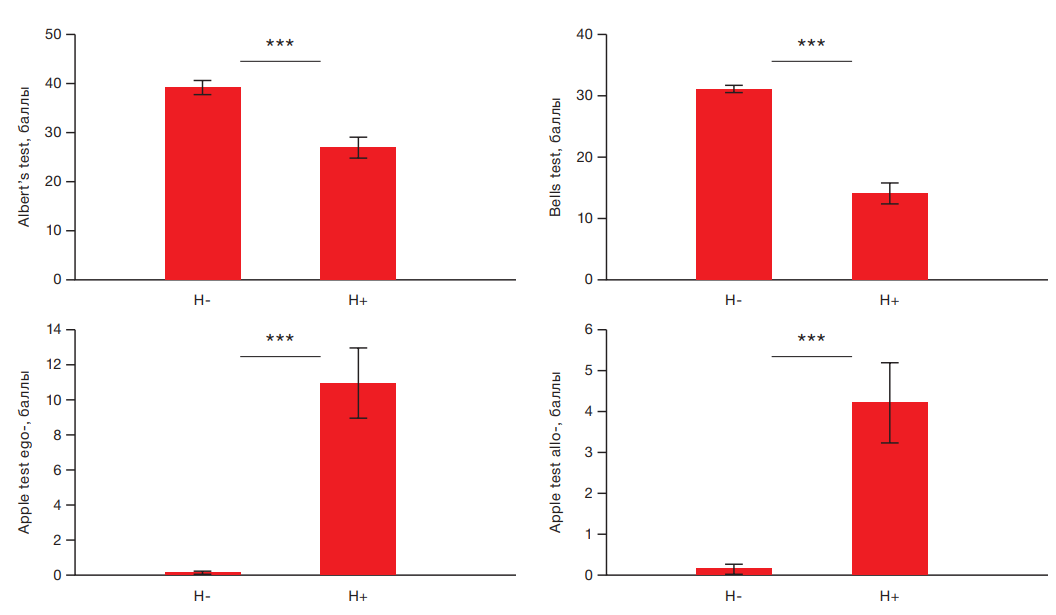
Figure prepared by the authors using their own data
Fig. 2. Intergroup comparisons of patients without (H–) and patients with (H+) neglect on each of the neuropsychological tests
Note: the data is presented as the average value and the error of the average value M ± m; *** — p < 0.001 is the level of statistical significance according to the Mann–Whitney test.
Table 3. Correlation analysis of the results of neuropsychological tests and eye tracking diagnostics
|
Tests name |
Albert’s test |
Bells test |
Line bisection test |
Apple test ego- |
Apple test allo- |
|
Albert’s test |
|
|
|
|
|
|
Bells test |
0.735 р < 0.001 |
|
|
|
|
|
Line bisection test |
–0.701 р < 0.001 |
–0.537 р = 0.004 |
|
|
|
|
Apple test ego- |
–0.526 р = 0.004 |
–0.647 р < 0.001 |
0.538 р = 0.010 |
|
|
|
Apple test allo- |
–0.003 р = 0.986 |
0.114 р = 0.564 |
0.131 р = 0.563 |
0.024 р = 0.904 |
|
|
Visual search on the eye tracker |
–0.422 р = 0.025 |
–0.613 р < 0.001 |
0.313 р = 0.166 |
0.370 р = 0.090 |
0.392 р = 0.072 |
Table prepared by the authors using their own data
Note: Spearman correlation coefficients (rs) are presented; p is the level of statistical significance.
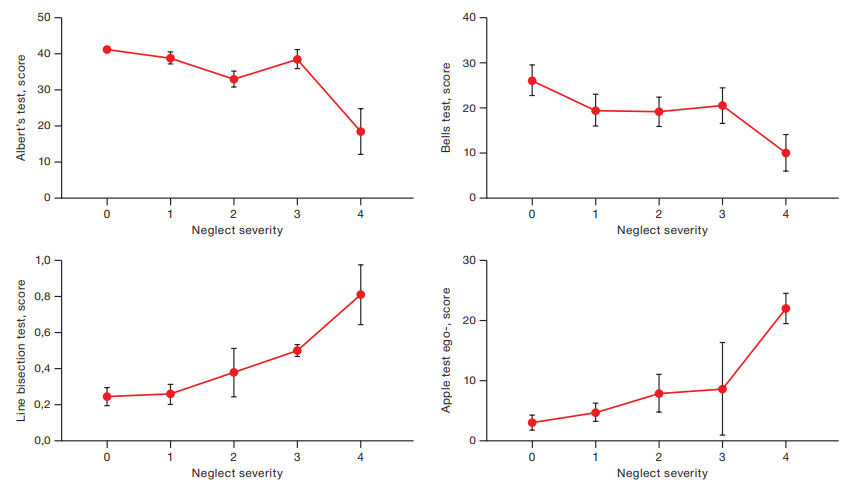
Figure prepared by the authors using their own data
Fig. 3. Dependence of the results of neuropsychological tests on the neglect severity
Note: the data are presented in the form of an average value and an error of the average value M ± m; the abscissa scale is the degree of severity of the defect: 0 — absent; 1 — mild, 2 — moderate, 3 — moderate-severe, 4 — severe.
DISCUSSION
In this study, we evaluated the diagnostic capabilities of classical neuropsychological tests (AT, BT, ApT, and LBS) and the eye tracking method for detecting neglect syndrome in stroke patients. A number of studies showed that detection of neglect syndrome should rely on the use of several different tests (crossing out, dividing lines in half, hardware and computerized methods) [1], which relates to the heterogeneity of the manifestation of this syndrome [18]. We determined a different level of sensitivity of these tests: thus, AT detected neglect syndrome only in 40% of patients in our sample, while the detection sensitivity of LBS was 93%.
Our results demonstrate that the determination of the neglect syndrome according to the established thresholds of each of the neuropsychological tests allows, including from a statistical point of view, the groups of patients with and without neglect to be reliably differentiated.
One of the most interesting results to consider turned out the highest sensitivity of LBS in detecting neglect syndrome in our sample. The LBS form was presented vertically, while all other cancellation tests were presented horizontally. The patients needed to assess the middle of the line and put a vertical mark. A classic sign of neglect syndrome is considered to be a disorder of spatial perception along the lateral (left-right) axis, and deletion tests are aimed at identifying this spatial disregard. However, a number of studies are aimed at studying the perception of the vertical axis based on visual, postural, and tactile information in patients with neglect syndrome [9][19][20]. A stroke can affect two separate but adjacent neural networks, one of which encodes spatial information for the horizontal axis, and the other — for the vertical [19].
The systematic review reported in [21] showed that patients with neglect syndrome exhibit more pronounced vertical deviations from the standard and have an unstable body position in an upright position in the first 3–6 months after the stroke compared with patients without this syndrome. The majority of the papers included in this review reported that, in participants with neglect, the ratio of the direction of inclination of the vertical line relative to the reference mark was opposite to the side of the brain lesion (i.e., when assessing the true visual vertical, the patient’s mark was tilted to the left with injuries in the right hemisphere).
When performing the bisection test, patients rely on visual-vestibular information about the vertical position of the cancellation tests and the vertical mark of the middle of the line. As shown in the studies described above, their subjective sense of vertical is shifted to the left; therefore, they perceive the task form positioned vertically to be shifted to the left relative to the real vertical. As a result, the right part of the space expands in front of patients, and they perceive the right part of the lines, ignoring the left part. On this basis, patients mark the center to the right of the true center.
An important aspect of the high sensitivity of LBS is the absence of distractors and features of the stimulus: size, orientation, and quantity on the sheet.
Despite the relatively low sensitivity of the strikeout tests in our study, they revealed the difficulties of patients in finding objects on the left. This correlates with the results of visual search using the eye tracking technique, where BT and AT demonstrated significant correlations with the search task. Patients with a severe attention deficit on the left, found in cancellation tests, spend more time searching for stimuli on the tracker. The high reliable latency of searching for objects on the left side compared to the right, revealed on the eye tracker, confirms the presence of pronounced oculomotor scanning anomalies noted in previous studies [11].
Allocentric neglect is one of the manifestations of neglect syndrome, in which the patient does not perceive the contralateral side relative to the midline of the perceived object [7]. In our study, the results of patients in AT, demonstrating the presence of an allocentric neglect at a level close to statistically significant, correlate with the time spent searching for objects in a visual search task using an eye tracker. This may indicate that due to the established allocentric neglect, it took patients longer to analyze the stimulus space when searching for a target object, since they saw only half of each object, which made the process of identification more difficult.
The nature of the stroke is a factor influencing the performance of neuropsychological tests and the search task on the tracker. According to [22], the proportion of patients with ischemic stroke (IS) and hemorrhagic stroke (HS) is about 70–75% and 15%, respectively. In our sample, IS accounted for 73.6% of the cases. IS is characterized by localization of the lesion in the area of blood supply to the SMA, which is responsible for the blood supply to 2/3 of the outer surface of the hemispheres: the main part of the cortex of the frontal, parietal, and temporal lobes. These areas are part of the system related to human orientation to external stimuli (dorsal and ventral attention networks) [23]. Indeed, the neglect syndrome in IS is more frequent and more pronounced than in HS, which is explained by IS affecting the key brain structures responsible for attention and perception of space.
During the analysis of the data, we noted a significant influence of the factor of vision loss on the performance of LBS and the search task on the eye tracker, while its influence on the rest of the cancellation tests was recorded at the trend level. The finding requires a more detailed study due to the variability of the causes of visual impairment, taking into account age and clinical characteristics. When analyzing blank, computerized, and hardware methods, it is worth considering not only the influence of cortical disorders, but also analyzer systems. The study [24] established an association of neglect syndrome with age, the presence of concomitant diseases and deterioration of health before stroke. However, there are no large-scale studies that could offer a reliable understanding of neglect syndrome in clinical practice [24].
In the neuropsychological clinical practice, the following severity degrees of neglect syndrome are distinguished: severe, moderate, and mild. Objective data for differentiating the severity include the latency of searching for numbers in Schulte tables, the ability to notice object images, reading and writing. The level of criticism of the patient’s actions also plays an important role in differentiating the neglect severity. The clinical picture of neglect often includes anosognosia syndrome, as a result of which patients are not critical and do not realize their defect, thereby not attempting to explore the contralateral lesion space [25]. Therefore, we compared the neuropsychologist conclusions with sensitized tests for neglect. As a result of the data analysis, a significant relationship was observed between the performance of AT, ApT, and LBS (not significant for BT, but direct) and the neglect severity: the worse the patients performed the tests, the more pronounced the neglect severity was according to objective neuropsychological examination data. These findings form the basis for studying the sensitivity of ApT and LBS in neglect syndrome of various severity and establishing their quantitative thresholds in larger cohorts of patients.
CONCLUSION
Neglect syndrome is a common visuospatial disorder in stroke patients, which has a negative impact on the rehabilitation process, subsequent recovery, and return to normal life. Our study has shown the importance of combining standard neuropsychological tests with the eye-tracking method for diagnosing neglect syndrome in stroke patients. Eye tracking has shown promise for determining the presence of neglect syndrome, which warrants further studies.
References
1. Kerkhoff G, Rode G, Clarke S. Treating neurovisual deficits and spatial neglect. Clinical pathways in stroke rehabilitation. 2021;191–217. https://doi.org/10.1007/978-3-030-58505-1
2. Shurupova MA, Aizenshtein AD, Ivanova GE. Homonymous hemianopia and visual neglect: I — phenomenology, diagnosis. Physical and rehabilitation medicine, medical rehabilitation. 2022;4(4):244–58 (In Russ.). https://doi.org/10.36425/rehab112424
3. Buklina SB. Disorders of higher mental functions with damage to the deep and stem structures of the brain. Мoscow: MEDpress-inform; 2016 (In Russ.).
4. Heilman KM, Valenstein E. Mechanisms underlying hemispatial neglect. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 1979;5(2):166–70. https://doi.org/10.1002/ana.410050210
5. Williams L, Kernot J, Hillier SL, Loetscher T. Spatial neglect subtypes, definitions and assessment tools: a scoping review. Frontiers in neurology. 2021;12:742365. https://doi.org/10.3389/fneur.2021.742365
6. Esposito E, Shekhtman G, Chen P. Prevalence of spatial neglect post-stroke: A systematic review. Annals of Physical and Rehabilitation Medicine. 2021;64(5):101459. https://doi.org/10.1016/j.rehab.2020.10.010
7. Marsh EB, Hillis AE. Dissociation between egocentric and allocentric visuospatial and tactile neglect in acute stroke. Cortex. 2008; 44(9):1215–20. https://doi.org/10.1016/j.cortex.2006.02.002
8. Terruzzi S, Albini F, Massetti G, Etzi R, Gallace A, Vallar G. The neuropsychological assessment of unilateral spatial neglect through computerized and virtual reality tools: a scoping review. Neuropsychology Review. 2024; 34(2):363–401. https://doi.org/10.1007/s11065-023-09586-3
9. Kerkhoff G. Multimodal spatial orientation deficits in left-sided visual neglect. Neuropsychologia. 1999;37(12):1387–405. https://doi.org/10.1016/S0028-3932(99)00031-7
10. Buslovich EV, Kulesh AA, Semashkova TD. Studying of method’s psychometric status of diagnostics unilateral spatial neglect. Social Sciences and Humanities Theory and Practice. 2018;1(2):764–74 (In Russ.). EDN: VPJSPG
11. Kaufmann BC, Cazzoli D, Pflugshaupt T, et al. Eyetracking during free visual exploration detects neglect more reliably than paper-pencil tests. Cortex. 2020;129:223–35. https://doi.org/10.1016/j.cortex.2020.04.021
12. Albert ML. A simple test of visual neglect. Neurology. 1973;23(6):658. https://doi.org/10.1212/WNL.23.6.658
13. Gauthier L, et al. The bells test: a quantitative and qualitative test for visual neglect. International journal of clinical neuropsychology. 1989;11(2):49–54.
14. Schenkenberg T, Bradford DC, Ajax ET. Line bisection and unilateral visual neglect in patients with neurologic impairment. Neurology. 1980;30(5):509. https://doi.org/10.1212/WNL.30.5.509
15. Bickerton WL, et al. Separating forms of neglect using the Apples Test: validation and functional prediction in chronic and acute stroke. Neuropsychology. 2011;25(5):567. https://doi.org/10.1037/a0023501
16. Jang H, Jang JS. Standardization of apple cancellation test for neglect patients in Korea: An observational study. World Journal of Clinical Cases. 2023;11(22):5236. https://doi.org/10.12998/wjcc.v11.i22.5236
17. Kunka B, Kostek B. Exploiting audio-visual correlation by means of gaze tracking. International Journal of Computer Science and Applications. 2010;7(3):104–22.
18. Grigoryeva VN, Semaka MA, Sorokina TA. Neglect in patients with acute non-lacunar hemispheric ischemic stroke: clinical subtypes, their incidence and association with the lesion localization. Medical Almanac. 2024;2(79):67–75 (In Russ.).
19. Pouget A., Driver J. Relating unilateral neglect to the neural coding of space. Current opinion in neurobiology. 2000;10(2):242–9. https://doi.org/10.1016/S0959-4388(00)00077-5
20. Dai S, et al. Lateropulsion after hemispheric stroke: a form of spatial neglect involving graviception. Neurology. 2021;96(17):e2160–71. https://doi.org/10.1212/WNL.0000000000011826
21. Embrechts E, et al. Association between spatial neglect and impaired verticality perception after stroke: A systematic review. Annals of Physical and Rehabilitation Medicine. 2023;66(3):101700. https://doi.org/10.1016/j.rehab.2022.101700
22. Bots ML, et al. γ-Glutamyltransferase and risk of stroke: the EUROSTROKE project. Journal of Epidemiology & Community Health. 2002;56(1):i25–9. https://doi.org/10.1136/jech.56.suppl_1.i25
23. Corbetta M, Shulman GL. Spatial neglect and attention networks. Annual review of neuroscience. 2011;34(1):569–99. https://doi.org/10.1146/annurev-neuro-061010-113731
24. Hammerbeck U, et al. Spatial neglect in stroke: Identification, disease process and association with outcome during inpatient rehabilitation. Brain sciences. 2019;9(12):374. https://doi.org/10.3390/brainsci9120374
25. Neglect syndrome in post-stroke patients and the possibilities of neuropsychological rehabilitation. Proceedings of the VII Siberian Psychological Forum, Tomsk; 2017.
About the Authors
A. D. AizenshteinRussian Federation
Alina D. Aizenshtein
Moscow
M. A. Shurupova
Russian Federation
Marina A. Shurupova, Cand. Sci. (Biol.)
Moscow
S. A. Eneeva
Russian Federation
Salima A. Eneeva
Moscow
G. E. Ivanova
Russian Federation
Galina E. Ivanova, Dr. Sci. (Med.), Professor
Moscow
Supplementary files
Review
For citations:
Aizenshtein A.D., Shurupova M.A., Eneeva S.A., Ivanova G.E. Identification of neglect syndrome in cerebral stroke patients using standard tests and eye tracking method. Extreme Medicine. 2025;27(2):161-168. https://doi.org/10.47183/mes.2025-308

















