Scroll to:
Modern approach in microsurgical elimination of tongue defects using computerized digital planning
https://doi.org/10.47183/mes.2024-26-3-98-105
Abstract
Introduction. The treatment of malignant neoplasms of the oral mucosa implies a combined treatment, whose first stage generally involves surgery. However, the most common non-personalized surgical methods are based on resection of the tongue, often affecting more than half of the organ, which can lead to significant functional deficiency and disability of patients.
Objective. To demonstrate the possibility of tongue defect reconstruction using preoperative computer 3D planning through clinical cases.
Маterials and methods. From 2021 to 2024, four patients with primary cancer of the lateral surface of the tongue were operated on using this methodology at the Maxillofacial Surgery Department of the NMICO FMBA of Russia. All patients underwent hemiglossectomy and preventive cervical lymphadenectomy on the affected side, with simultaneous reconstruction of the tongue using a radial forearm flap. The average age of the patients was 53 years; males outnumbered females by a ratio of 3:1. Patients presented with stages rT1-rT4; histological examination revealed no regional lymph node involvement (N0) in any patient. Preoperative instrumental examinations included: magnetic resonance imaging (MRI) of the soft tissues of the maxillofacial area with contrast enhancement; multislice computed tomography (MSCT) of the maxillofacial area with contrast enhancement; MSCT of the donor area (forearm) with contrast enhancement; Doppler ultrasound of the brachiocephalic trunk vessels and donor area vessels; transnasal endoscopic laryngoscopy with swallowing tests (three-swallow test) with video recording. All patients were surveyed preoperatively and postoperatively using EORT QLQ — H&N35, EORT QLQ — C30, FACT– H&N, MD Anderson, and VHI-10 questionnaires. Patients with abundant hair in the donor area underwent laser hair removal prior to hospitalization. After performing computer simulation of the surgical intervention using Slicer and Blender software, templates were printed on a Elegoo Saturn 2 printer. Assessment of speech and swallowing functions was carried out by a speech therapist specializing in these areas using the Pokrovsky protocol and Vospector-DSI software at both preoperative and postoperative stages. The attending physician performed anthropophotometry and video recording of patient complaints and speech at all stages of care. The postoperative period was without complications; nasogastric tubes were removed on the 12th day; the average hospital stay was 14 days.
Results. The flap survival rate was 100% across the entire series of observations. Oncological radicality was achieved at R0 for all patients. The average duration of the surgical intervention was 288 minutes. In three patients, the acoustic parameters of speech were within normal limits (in one patient, this parameter could not be assessed due to systemic speech underdevelopment caused by hearing impairment). The average syllable intelligibility coefficient according to Pokrovsky was 88%. All patients adapted to their usual diet and continued their professional activities. According to the results of the EORT QLQ — H&N35, EORT QLQ — C30, and FACT — H&N questionnaires, patients rated their quality of life as good in one case and excellent in three cases.
Conclusions. The developed algorithm for preoperative computer planning is promising. The use of surgical templates allowed for adequate oncological radicality, synchronized the simultaneous work of two surgical teams, reduced the duration of anesthetic assistance (with an average surgical intervention time of 288 minutes), and achieved good functional and aesthetic results. However, this methodology requires further refinement in a larger group of patients.
Keywords
For citations:
Khachatryan A.A., Nazarian D.N., Chernenkiy M.M., Dzhuganova V.О., Fedosov A.V., Zakharov G.K., Potapov M.B., Danishuk O.I., Osipenko E.V., Micheeva E.I. Modern approach in microsurgical elimination of tongue defects using computerized digital planning. Extreme Medicine. 2024;26(3):98-105. https://doi.org/10.47183/mes.2024-26-3-98-105
INTRODUCTION
Malignant neoplasms (MN) of the head and neck occupy the sixth place in the structure of general oncologic morbidity; in 90% of cases, MNs are presented by squamous cell cancer. Of cancers in the head and neck region, oral cancer is the most commonly occurring malignant neoplasm. The leading localization of all tumor formations of the oral cavity in 60% of cases is the tongue with the same frequency of lesions of both the right and left halves of the tongue [1-3]. In the structure of oncologic diseases in the period 2013–2020 in Russia, the incidence of oral mucosal tumors amounted to about 1.9% according to different sources [4].
One of the main approaches for the treatment of malignant neoplasms of the oral mucosa at the first stage involves surgery. However, resection of even a part of the tongue significantly affects processes of swallowing and speech formation, resulting in a functional reduction in quality of life [5–10]. The current state of the art in the treatment of patients with tongue defects involves the use of free revascularized flaps on microvascular anastomoses [5][10][11].
In 1981, Yang described a method of using radial fasciocutaneous forearm flap to repair defects in various areas of the human body. This method has steadily taken its place in the arsenal of reconstructive surgeons. A flap is a thin plastic material with a permanent vascular anatomy and a long vascular pedicle. In tongue reconstruction, the flap is used for defects that form following hemiglossectomies; in order to increase its volume, it can be provided with an additional amount of adipose tissue harvested from the patient’s forearm. Moreover, sensitive reinnervation of the flap can be accomplished at the expense of the forearm cutaneous nerve [12].
Many techniques for cutting a forearm cutaneous fascial flap (bilobed flap) and adapting the flap to the defect edges have been described [13]. However, these methods cannot be called personalized due to the impossibility of subjecting them to mathematical analysis and obtaining adequate information about the required flap parameters. The use of digital technologies in reconstructive surgery of the tongue makes it possible to obtain a predictable and standardized result, contributing to the reduction of the operative time of intervention due to the possibility of simultaneous work of two teams [14].
The use of intraoperatively cut resection 2D-templates, most often on paper, when planning soft tissue autografts, has its disadvantages, including the impossibility of designing the template in advance due to the template’s creation following excision of the tumor mass and visualization of the tongue defect based only on the visual control of the surgeon. This moment causes prolongation of anesthesiologic and surgical aids due to the impossibility of simultaneous work of two surgical teams. Another disadvantage of the 2D technique is also due to a lack of information at the preoperative stage about the planned volume of tongue resection and tumor size. This is due to the impossibility of assessing the subsequent loss of tongue volume associated with radiation therapy and/or flap atrophy prior to surgical intervention [15–16]. To solve this problem, we tested the proposed method of tongue defect repair with a soft tissue flap in cancer patients requiring tongue resection. The approach involves one-stage tongue reconstruction based on 3D computer planning and creation of resection templates. Scientific novelty is confirmed by the Russian patent for invention No.2024104882 “Method of tongue defects elimination after partial glossectomy”, published on 07/04/2024.
The study purpose was to demonstrate on a series of clinical cases the possibility of tongue defect repair using preoperative computerized 3D planning.
МАТЕRIALS AND METHODS
From 2021 to 2024, 4 patients (three men and one woman) diagnosed with primary cancer of tongue lateral surface were operated on at the Maxillofacial Surgery Department of the “National Medical Research Center for Otorhinolaryngology of the Federal Medical and Biological Agency” using a microsurgical tongue defect repair technique based on 3D computerized digital planning. Patients were presented with stages of tumor process development pT1-pT4a, without regional lymph node involvement (N0), confirmed by the results of histological examination. The average age of the patients was 53 years. All patients underwent hemiglossectomy and preventive lymphodissection on the side of the lesion with one-stage reconstruction of the tongue with a radial forearm flap. The patients’ summary data are shown in Table 1.
Instrumental methods of research at the preoperative stage included:
- magnetic resonance imaging of soft tissues of the maxillofacial region with contrast enhancement (MRI of the maxillofacial region with contrast) to clarify the stage of the process according to the T-criterion (international classification of oncological tumors) and assess the spread of the tumor process in the tissues of the tongue;
- multispiral computed tomography of the maxillofacial region with contrast enhancement to select recipient vessels;
- determination of the vascular flow of the external carotid artery basin and exclusion of intravascular pathologies (occlusion, thrombosis);
- multispiral computed tomography of the donor area (forearm) with contrast enhancement (MSCT with contrast enhancement) to take into account the diameter of the main trunk vessels, to detect anomalies of the vascular channel and anatomical features of the vessels;
- Doppler ultrasound of the brachiocephalic trunk vessels and vessels of the donor area.
To select the donor area (upper extremity of the forearm), a clinical assessment of arterial patency and collateral blood supply of the hand by Allen test was performed. To assess swallowing function, transnasal endoscopic laryngoscopy with swallowing tests (three-glottic test) with video recording was performed in all patients.
All patients at the preoperative and postoperative stages were surveyed using quality of life questionnaires recommended by the European Organization for Research and Treatment of Cancer (EORTC) for head and neck module (QLQ-H&N35), (EORTC Quality of Life Questionnaire). The questionnaire additionally included MD Anderson and Voice Handicap Index (VHI-10) scales, which have higher specificity for patients treated for oropharyngeal cancer. The questionnaires were administered at prehospital and at each follow-up visit after 1, 3, 6, and 12 months. Patients with abundant hair in the donor area underwent laser hair removal at the prehospital stage. Speech and swallowing functions were assessed by a staff phoniatrician (speech and swallowing specialist) using the Pokrovsky protocol and Vospector-DSI software at the preoperative and postoperative stages [19]. The attending physician performed anthropophotometry and video recording of patients’ speech and complaints at all stages of the curation. Treatment tactics for all patients were determined at the oncologic consilium on the basis of the A.I. Burnazyan Federal Medical Biophysical Center.
Computer modeling of the surgical intervention was performed using Slicer and Blender software; the templates were printed on a Formlab 3 3D printer.
Table 1. Summary data of patients
|
Patient data |
Patients |
|||
|
1 |
2 |
3 |
4 |
|
|
Gender |
Male |
Male |
Male |
Female |
|
Age, years |
40 |
50 |
50 |
70 |
|
Location of tumor |
Right lateral surface of the tongue |
Left lateral surface of the tongue |
Right lateral surface of the tongue, root of the tongue |
Right lateral surface of the tongue |
|
Stage of tumor process according to TNM* |
рТ2N0M0 |
рТ2N0M0 |
рТ4аN0M0 |
рТ1N0M0 |
|
Resection feature |
Resection of the right lateral surface of the tongue with preservation of the tongue tip and root |
Resection of the left lateral surface of the tongue with preservation of the tongue tip and root |
Resection of the right lateral surface, tip and root of the tongue |
Resection of the right lateral surface of the tongue with preservation of the tongue tip and root |
|
Percentage of resected volume from tongue volume, % |
40 |
40 |
60 |
40 |
|
Flap dimensions length/width, mm |
50/40 |
57/72 |
71/65 |
60/40 |
|
The timing of flap collection, min |
125 |
115 |
90 |
130 |
|
Resection time, min |
80 |
92 |
97 |
82 |
|
Time of surgical intervention, min |
310 |
270 |
295 |
280 |
|
Hospitalization time, days in hospital |
13 |
14 |
15 |
14 |
|
Period of nasogastric tube removal, days |
12 |
12 |
12 |
12 |
|
Pokrovsky index, % |
93 |
_ |
73 |
95 |
|
Postoperative complications |
Venous stasis of the flap |
no |
no |
no |
|
Observation period, months |
21 |
16 |
16 |
6 |
|
Oncologic status |
Relapse-free course |
Relapse-free course |
Relapse-free course |
Relapse-free course |
|
Patient/s status at the moment of article publication |
alive |
alive |
alive |
alive |
|
Self-questionnaire quality of life assessment (1 to 7 points) |
6 (good) |
6 (good) |
6 (good) |
7 (excellent) |
Table prepared by the authors using their own data
Note: * — TNM (international classification of oncological tumors, where T — tumor, the prevalence of the primary tumor, N (nodus) the presence, absence and advance of metastases in regional lymph nodes, M (detached metastases), the presence or absence of detached metastases.
RESULTS
One week before the surgical intervention, computerized preoperative planning was carried out based on the data of the MSCTs of the maxillofacial region upper extremities, as well as the MRI of the maxillofacial region. For this purpose, tongue tissues were contoured slice-by-slice with a step of 5–7 slices.
Further on the basis of mathematical interpolation methods using Slicer and Blender software the selected volume of the formation was determined taking into account the indentation from the tumor borders of 1.5 cm to reach the edges of the resection borders R0. The obtained data were converted to surface area and adapted to the topography of the donor arm by placing the surface of the stencil template over the axial vessels (radial vessels) to incorporate them into the flap. The surface area of the flap was increased by 15% taking into account possible flap shrinkage after radiation therapy. Thus, two templates were made: a resection template for hemiglossectomy and a template for cutting the skin area of the radial flap (Fig. 1).
Following coordination of preoperative planning with the operating surgeons, the digital project in the form of an STL (stereolithographic) model was sent for printing on an Elegoo Saturn 2 3D printer. The average time of template printing was 40–50 min.
Surgical interventions were performed by two teams of surgeons according to the standard protocol. The first team of surgeons performed tongue tumor ablation using a resection template, cervical lymphodissection, and isolation of recipient vessels of the neck (Fig. 2).
Each patient underwent emergency intraoperative edge biopsy (6 preparations) of the resection, in all cases the resection edges were R0 (Fig. 3).
The second team of surgeons simultaneously isolated the radial flap using a template. The average time of the resection stage was 87 min. The average time of flap harvesting was about 115 min. Radial flap isolation in all cases was performed with inclusion of the radial artery and vena comitans, as well as the lateral cutaneous nerve of the forearm (Fig. 4). Following flap isolation, the vascular pedicle of the graft was cut off and the graft was moved into the oral cavity.
After affixing the skin site of the flap to the remaining part of the tongue with guiding sutures, the donor vessels were carried out in a tunnel formed in the soft tissues of the floor of the mouth, after which the microsurgical stage was performed. Anastomosing of the radial artery with the facial artery was performed in all cases according to the type of “end-to-end” anastomosis; similarly, vena comitans were anastomosed with the external jugular vein. At the final stage, neurorrhaphy of the lateral cutaneous nerve and lingual nerve was performed in two cases, while neurorrhaphy of the hyoid nerve (end-to-side type) was also carried out in two cases. The average time of the microsurgical stage was 45 min. After restarting the blood flow, the filling of the donor vessels was assessed visually and using a portable Doppler Minidop (Bioss). When the flap had been successfully adapted to the remaining part of the tongue with resorbable Vicryl 3.0 thread, layer-by-layer wound closure was performed (Fig. 5).
The postoperative period in most patients was uneventful. Only one patient had venous stasis of the flap 3 hours after the surgical intervention; in this case, a revision surgery with repeated venous anastomoses was performed. The postoperative period passed further in this patient without peculiarities. The nasogastric tube was removed in all patients on the 12th day; the average period of hospitalization was 14 days (Fig. 6).
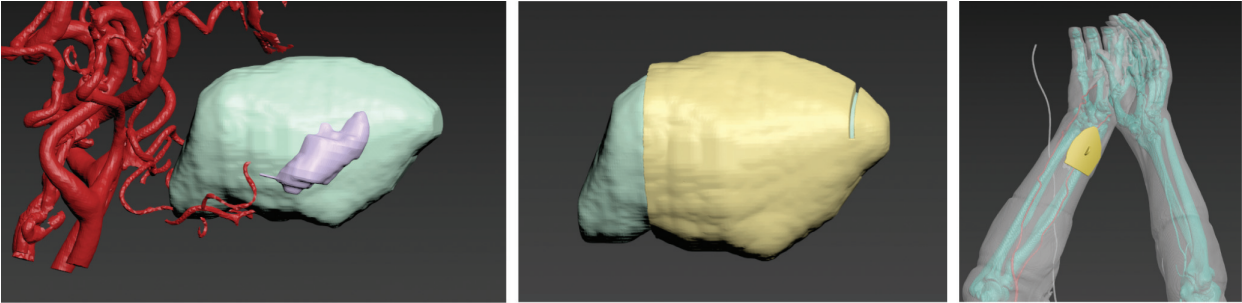
Figure prepared by the authors
Fig. 1. Preoperative 3D computer planning
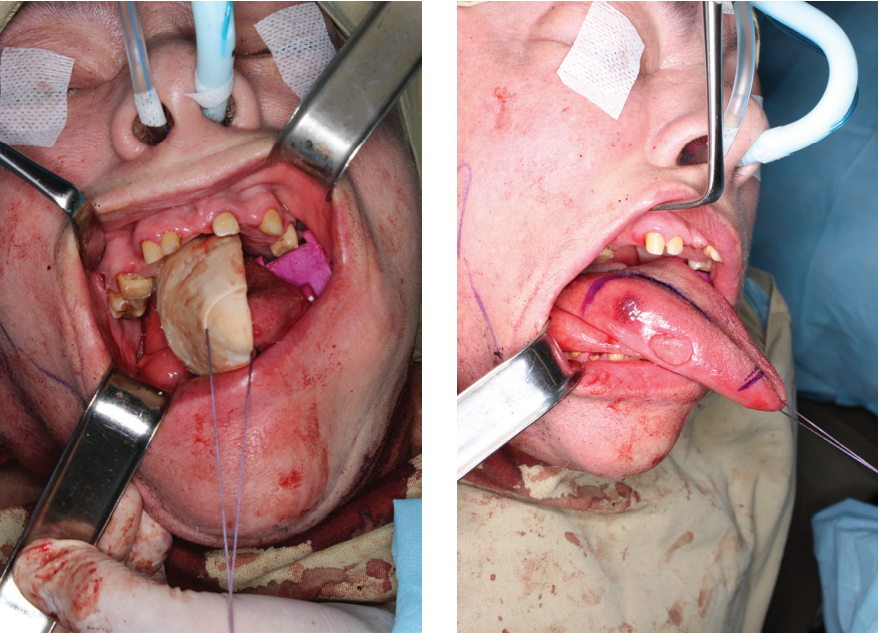
Figure prepared by the authors
Fig. 2. Marking the resection area using a resection template for visualizing a malignant neoplasm of the tongue affecting its lateral surface
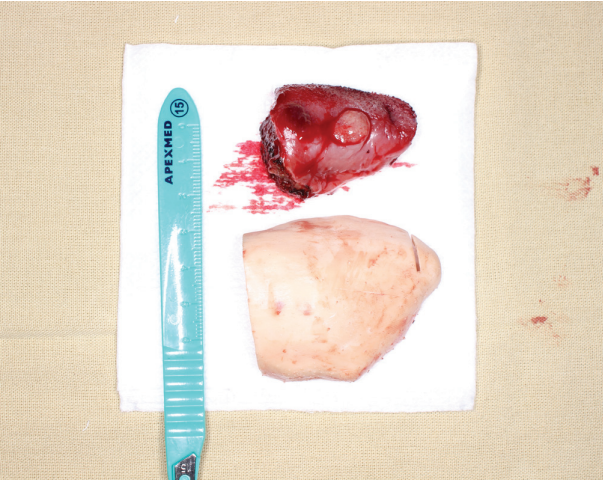
Figure prepared by the authors
Fig. 3. Removed tongue preparation
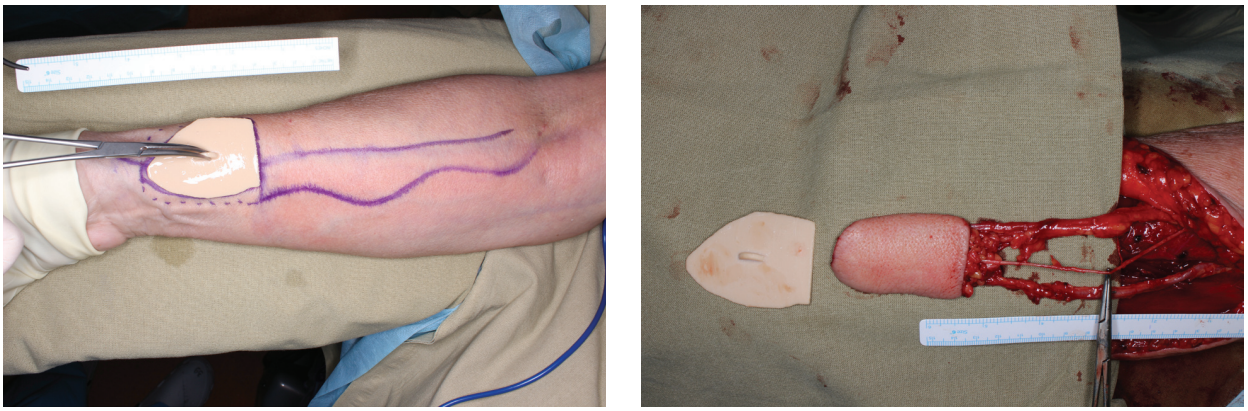
Figure prepared by the authors
Fig. 4. Marking a flap using a template. Radial flap on a vascular pedicle

Figure prepared by the authors
Fig. 5. View of the flap after suturing the wound and restarting the blood flow
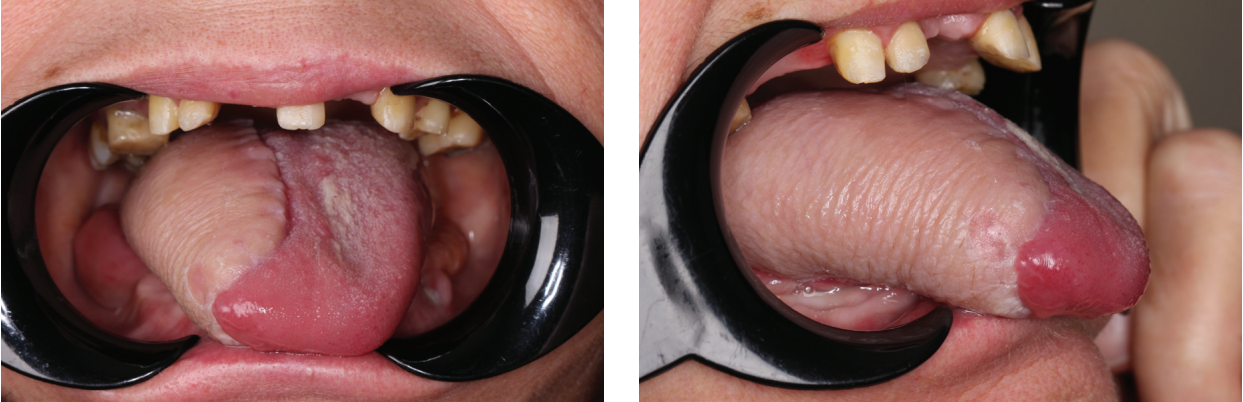
Figure prepared by the authors
Fig. 6. Anthropophotometry one month after surgery
DISCUSSION
Computer modeling is widely used in reconstructive maxillofacial surgery to eliminate bone defects of the maxillofacial region to facilitate the performance of complex reconstructive surgeries with a predictable result. However, in the elimination of soft tissue defects of the maxillofacial region, the use of surgical templates remains poorly studied. The complexity of applying this technique and planning soft tissue autografts lies in the absence of stable supporting bone elements, as well as the need to not only restore the volume of tissues, but also to ensure their proper mobility [14].
The first use of resection templates — namely, resection 2D-templates in the planning of soft tissue autografts for replacing the deficit of tongue tissues — was first described by R.M. Baskin et al. [15].
It should be noted that the results of the application of computerized planning and template surgery for the elimination of soft tissue defects of the tongue and the floor of the mouth are not described in the Russian scientific literature; in the foreign literature, we found only two original articles covering this issue [16–17].
The closest approach to the one tested by us is that presented by H. Koumoullis, who first proposed a method of using 3D modeling and template surgery to perform tongue reconstruction following glossectomy using Personalized Patient-specific Planning of Soft Tissue Reconstruction (PANSOFOS) [16]. The author noted the possibility of personalized reconstruction of soft tissues of the head and neck with a soft tissue autograft using 3D-planning. However, the main disadvantage of his proposed technique consisted in an inability to predict the planned volume of tongue resection at the preoperative stage or to determine the loss of organ volume after radiation therapy and/or flap atrophy.
Lu H, Qin J, Yue R, Liu C et al describe a method of tumor visualization using computed tomography data to perform precision resection of midline tongue tumors without disturbing blood flow through the facial arteries. However, this technique did not involve the use of surgical templates [17].
Sinha P et al proposed a method of tongue tumor visualization by printing a physical model of the patient’s tongue on a 3D printer with an alternative color of the tumor at the preoperative stage, allowing surgeons to carry out a better assessment of the extent of tumor spread. However, this approach did not include the fabrication of either resection templates or templates for free flap cutting [18].
In approbation of the above approach (preoperative planning of soft tissue reconstructive autografts), we and a number of authors [19] noted a significant decrease in the time of surgical intervention, which significantly reduces intraoperative risks for the patient and reduces the financial costs of anesthesia care.
The described approach to tongue defect elimination following removal of malignant neoplasm using computer-aided digital planning, which is based on previously performed surgical intervention in the digital field, can be used to accurately (with an error of 0.2 mm) determine the boundaries of the tumor. To ensure the required oncologic radicality (clean margins), the resection template includes a parameter such as an oncologic margin of 1.5 cm from the tumor. The stencil for the cutaneous fascial flap pattern, which takes into account the volume of the resected part of the tongue, has an increased volume of 15% to level out postoperative scarring and reduce flap volume.
Despite the availability of modern protocols for suppressing artifacts from metal prosthetic restorations during head and neck radiology, not all patients were able to achieve objective visualization of the soft tissues of the tongue and floor of the oral cavity. Most of our patients had metal orthopedic constructions (gold, cobalt-chromium alloy) in the oral cavity at the time of treatment. In order to level out artifacts in radial methods of diagnostics (MRI, MSCT) and following a clinical examination of the oral cavity, the staff dentist-orthopedist removed all metal prosthetic constructions and replaced them with plastic crowns.
The problem of tongue mobility and changes in its volume due to muscle contraction at the stage of radial diagnosis remains a significant problem, whose solution will be presented in subsequent studies. In order to standardize preoperative planning, the need to create specialized protocols for the position of the tongue in the oral cavity at the diagnostic stages seems
relevant.
CONCLUSIONS
The proposed 3D computerized planning method has demonstrated its utility in achieving accurate preoperative surgical planning. The use of surgical templates to achieve adequate oncological radicality (due to the pre-planned resection zone), synchronization of the work of two surgical teams, and reduction of the anesthesia time (average time of surgical intervention 288 min) demonstrates good functional and aesthetic results. The resection template provides a means for neoplasm removal in accordance with oncological principles; the template-pencil is used to accurately mark the shape and volume of the free microsurgical flap to in order to eliminate the tongue defect. However, due to the mobility of the tongue and the variability of its shape, new protocols for preoperative instrumental diagnostics are required for standardizing the position of the organ in the oral cavity. Thus, due to the need to develop new reconstructive operations to improve functional and reduce traumatization without compromising oncologic radicality, the presented surgical intervention approach represents a promising direction requiring further refinements and approbation on a larger group of patients.
References
1. Sarode G, Maniyar N, Sarode SC, Jafer M, Patil S, Awan KH. Epidemiologic aspects of oral cancer. Dis Mon. 2020;66(12):100988. https://doi.org/10.1016/j.disamonth.2020.100988
2. Kumar M, Nanavati R, Modi TG, Dobariya C. Oral cancer: Etiology and risk factors: A review. J Cancer Res Ther. 2016;12(2):458–63. https://doi.org/10.4103/0973-1482.186696
3. Stepan KO, Mazul AL, Larson J, Shah P, Jackson RS, Pipkorn P, et al. Changing Epidemiology of Oral Cavity Cancer in the United States. Otolaryngol Head Neck Surg. 2023;168(4):761–8. https://doi.org/10.1177/01945998221098011
4. Rychlevich AA. Total incidence of oral mucosal malignancies in the Russian Federation in 2013–2020. Current problems of health care and medical statistics. 2022;4:689–705 (In Russ.). https://doi.org/10.24412/2312-2935-2022-4-689-705
5. Yi CR, Jeong WS, Oh TS, Koh KS, Choi JW. Analysis of speech and functional outcomes in tongue reconstruction after hemiglossectomy. Journal of Reconstructive Microsurgery. 2020;36:507–13. https://doi.org/10.1055/s-0040-1709493
6. Engel H, Huang JJ, Lin CY, Lam W, Kao HK, Gazyakan E, Cheng MH. A strategic approach for tongue reconstruction to achieve predictable and improved functional and aesthetic outcomes. Plast Reconstr Surg. 2010;126(6):1967–77. https://doi.org/10.1097/PRS.0b013e3181f44742
7. Lam L, Samman N. Speech and swallowing following tongue cancer surgery and free flap reconstruction--a systematic review. Oral Oncol. 2013;49(6):507–24. https://doi.org/10.1016/j.oraloncology.2013.03.001
8. Chang EI, Yu P, Skoracki RJ, Liu J, Hanasono MM. Comprehensive analysis of functional outcomes and survival after microvascular reconstruction of glossectomy defects. Ann Surg Oncol. 2015;22(9):3061–9. https://doi.org/10.1245/s10434-015-4386-6
9. Ihara Y, Tashimo Y, Nozue S, Iizumi Y, Fukunishi Y, Saito Y, Shimane T, Takahashi K. Changes in Oral Function and Quality of Life in Tongue Cancer Patients Based on Resected Area. Asian Pac J Cancer Prev. 2021;22(8):2549–57. https://doi.org/10.31557/APJCP.2021.22.8.2549
10. Gilbert RW. Reconstruction of the oral cavity; past, present and future. Oral Oncol. 2020;108:104683. https://doi.org/10.1016/j.oraloncology.2020.104683
11. Haughey BH. Tongue reconstruction: concepts and practice. Laryngoscope. 1993;103(10):1132–41. https://doi.org/10.1288/00005537-199310000-00010
12. Chepeha DB, Teknos TN, Shargorodsky J, Sacco AG, Lyden T, Prince ME, Bradford CR, Wolf GT. Rectangle tongue template for reconstruction of the hemiglossectomy defect. Arch Otolaryngol Head Neck Surg. 2008;134(9):993–8. https://doi.org/10.1001/archotol.134.9.993
13. Absolon KB, Rogers W, Aust JB. Some historical developments of the surgical therapy of tongue cancer from the seventeenth to the nineteenth century. Am J Surg. 1962;104:686–91. https://doi.org/10.1016/0002-9610(62)90419-1
14. Jacek B, Maciej P, Tomasz P, Agata B, Wiesław K, Radosław W, et al. 3D printed models in mandibular reconstruction with bony free flaps. J Mater Sci Mater Med. 2018;29(3):23–5. https://doi.org/10.1007/s10856-018-6029-5
15. Baskin RM, Seikaly H, Sawhney R, Danan D, Burt M, Idris S, et al. Tongue reconstruction: Rebuilding mobile three-dimensional structures from immobile two-dimensional substrates, a fresh cadaver study. Head Neck. 2019;41(10):3693–99. https://doi.org/10.1002/hed.25889
16. Koumoullis H, Burley O, Kyzas P. Patient-specific soft tissue reconstruction: an IDEAL stage I report of hemiglossectomy reconstruction and introduction of the PANSOFOS flap. Br J Oral Maxillofac Surg. 2020;58(6):681–6. https://doi.org/10.1016/j.bjoms.2020.04.017
17. Lu H, Qin J, Yue R, Liu C, Li S, Wu D. Application of 3D reconstruction for midline glossectomy in OSA patients. Eur Arch Otorhinolaryngol. 2020;277(3):925–31. https://doi.org/10.1007/s00405-020-05783-5
18. Sinha P, Bylapudi BP, Puranik P, Subash A, Rao V. 3D Patient-Specific Biomechanical Model of the Tongue for the Management of Tongue Tumors: Conceptualization to Reality. Sisli Etfal Hastan Tip Bul. 2022;56(4):559–63. https://doi.org/10.14744/SEMB.2022.37039
19. McCarty JL, Corey AS, El-Deiry MW, Baddour HM, Cavazuti BM, Hudgins PA. Imaging of Surgical Free Flaps in Head and Neck Reconstruction. AJNR Am J Neuroradiol. 2019;40(1):5–13. https://doi.org/10.3174/ajnr.A5776
20. Pokrovskii NB. Raschet i izmerenie razborchivosti rechi. Svyazizdat. 1962;392. (In Russ).
About the Authors
A. A. KhachatryanRussian Federation
Moscow
D. N. Nazarian
Russian Federation
Moscow
M. M. Chernenkiy
Russian Federation
Moscow
V. О. Dzhuganova
Russian Federation
Moscow
A. V. Fedosov
Russian Federation
Moscow
G. K. Zakharov
Russian Federation
Moscow
M. B. Potapov
Russian Federation
Moscow
O. I. Danishuk
Russian Federation
Moscow
E. V. Osipenko
Russian Federation
Moscow
E. I. Micheeva
Russian Federation
Moscow
Supplementary files
Review
For citations:
Khachatryan A.A., Nazarian D.N., Chernenkiy M.M., Dzhuganova V.О., Fedosov A.V., Zakharov G.K., Potapov M.B., Danishuk O.I., Osipenko E.V., Micheeva E.I. Modern approach in microsurgical elimination of tongue defects using computerized digital planning. Extreme Medicine. 2024;26(3):98-105. https://doi.org/10.47183/mes.2024-26-3-98-105

















