Scroll to:
Removal of a metal fragment and floating thrombus from the internal jugular vein of a serviceman in a field hospital
https://doi.org/10.47183/mes.2025-349
Abstract
Introduction. Fragment wounds of the neck with neurovascular bundle injury sustained during combat operations represent a relevant problem in the field of extreme medicine. High mortality rates, along with a lack of sufficient research, contribute to uncertainty in determining optimal treatment tactics.
Case report. A successful surgical treatment of a serviceman with a fragment wound to the neck caused by a foreign metallic body (shell fragment) involving the internal jugular vein and a floating thrombus was performed in a field hospital. An open surgery was conducted to remove the foreign metallic body and the floating thrombus from the internal jugular vein, followed by repair of the venous wall with a 7/0 polypropylene suture. The postoperative course was uneventful.
Conclusions. The presented case demonstrates previously unpublished data on a variant of fragment injury to the internal jugular vein. The proposed surgical technique has proven to be effective and safe.
Keywords
For citations:
Vasiliev D.S., Kazantsev A.N., Kolesnikov V.V., Yakimavichus R.P., Shishkin A.G., Belyai Zh.M., Tenishev R.R., Kholmatov V.V. Removal of a metal fragment and floating thrombus from the internal jugular vein of a serviceman in a field hospital. Extreme Medicine. 2025;27(4):500-504. https://doi.org/10.47183/mes.2025-349
INTRODUCTION
Military-field vascular surgery remains a relevant discipline within modern medicine of extreme situations. However, the existing literature lacks sufficient research dedicated to the surgical management of patients with vascular injuries sustained during combat operations. This trend can be traced back to the report by Oppel [1], published during World War I in 1915. At that time, military hospitals admitted rare patients with injuries to major arteries and veins due to high mortality from ongoing bleeding on the battlefield [1]. Consequently, the proportion of servicemen with such wounds did not exceed 1%, presenting as false aneurysms in 30% of cases and as hemorrhage in 70% [2].
According to Akhutin [3], until 1938, the most common surgical method for arterial and venous injuries in combat settings had been vessel ligation. Reconstructive surgeries became more widespread in military field hospitals during World War II. This shift was partially determined by the difficulty in evacuating casualties due to artillery shelling and the modernization of long-range weaponry. By April 1943, Petrovsky had performed 238 successful reconstructive procedures for major vascular injuries [4]. Among these, fragment wounds to the neck were of particular interest. The neck is the least protected body area, and bleeding from injuries to the brachiocephalic arteries and/or jugular veins cannot be controlled with a tourniquet on the battlefield, significantly reducing the wounded soldier’s chances of evacuation to specialized medical care facilities.
The first documented experience in surgical management of neck injuries in servicemen was published by Pirogov [5] during the Eastern War of 1853–1856. He emphasized the importance of urgent surgical intervention in this cohort of patients [5]. During World War II, neck wounds accounted for 9.63–19.2% of all injuries, with fragment wounds comprising 68.4–74.0% of cases [6]. These figures highlight the high vulnerability of this anatomical region.
Surgical treatment of fragment wounds to major neck vessels remains critically relevant in modern combat operations. However, the available literature contains only sporadic reports focusing primarily on arterial injuries and surgical management of false aneurysms [7][8]. This gap has resulted in the absence of a unified surgical approach for servicemen with injuries to the deep veins of the neck.
In this article, we report the outcome of surgical intervention in a patient with a fragment wound to the neck penetrating the left jugular vein and complicated by a floating thrombus.
CASE REPORT
A 28-year-old male serviceman sustained a fragment wound from an artillery shell explosion during a combat mission and was evacuated to a field hospital.
The patient’s condition was assessed using military field surgery (MFS) scoring systems:
- MFS-DS (Damage Severity Scale for MFS): 8.1 points — severe injury;
- Abbreviated Injury Scale: 4 points — critical injury;
- MFS-AS (Admission Severity Scale for MFS): 12 points — non-severe condition;
- Revised Trauma Score: 7.8408 points — non-severe condition.
Consciousness was clear (15 points on the Glasgow Coma Scale). Complaints included pain in the left shoulder and left side of the neck.
Local findings: A 2 cm lacerated wound on the posterior surface of the left shoulder with scant serosanguineous discharge (Fig. 1).
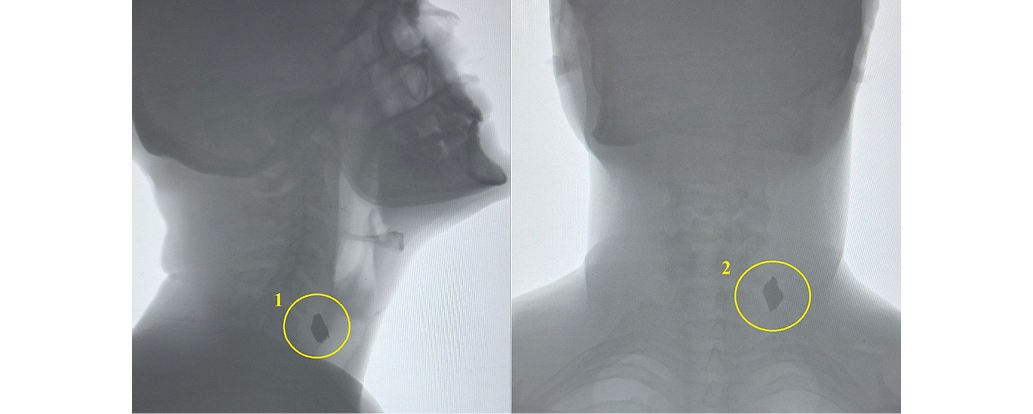
Neck radiography revealed a metallic foreign body (fragment) measuring 2x2 cm within the deep tissues of the left neck (Fig. 2).
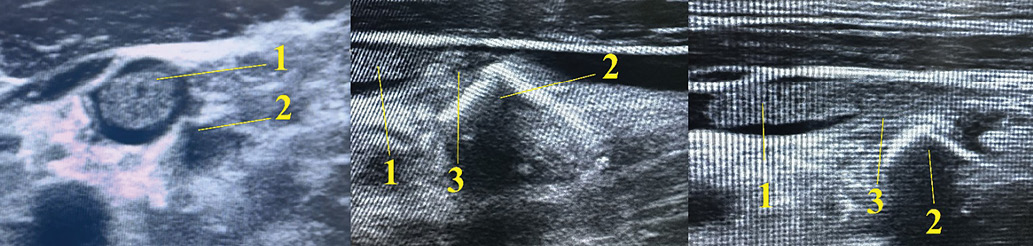
According to ultrasonography (USG), the fragment was located between the left common carotid artery and the internal jugular vein (IJV), penetrating the IJV. A 3 cm floating thrombus attached to the fragment was visualized within the IJV lumen (Fig. 3).
Diagnosis established: Combined fragment wound to the left neck and left upper extremity. A blind (non-penetrating) fragment wound to zone II of the left neck, resulting in injury to the internal jugular vein with formation of a floating thrombus. A blind fragment wound to the soft tissues of the left shoulder.
This injury is classified as severe according to the List of Injuries approved by Decree No. 855 of the Government of the Russian Federation
(29.07.1998)1.
The decision was made to perform surgical intervention comprising thrombectomy from the IJV with removal of the fragment (time from injury to surgery onset: 5 h).
Procedure: A longitudinal incision was made along the lateral border of the left sternocleidomastoid muscle. The IJV was isolated. A 1 cm defect in the posterior wall of the IJV was identified, caused by foreign body invasion — a metallic fragment.
Heparin was administered intravenously in the amount of 5000 IU. The IJV was clamped 3 cm distal and proximal to the defect. A 2 cm venotomy of the anterior IJV wall was performed. The thrombus was removed from its lumen. Subsequently, the foreign body was extracted (Fig. 4).
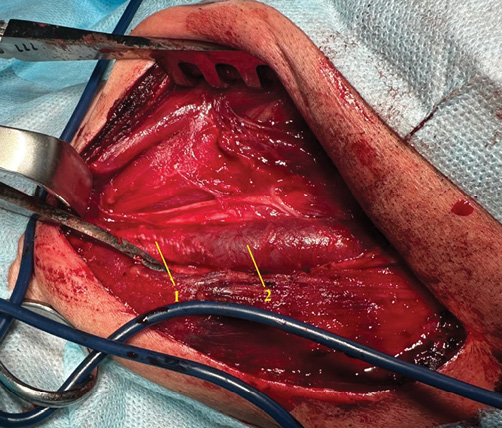
The defect in the posterior wall of the IJV was repaired using a 7/0 polypropylene suture. Subsequently, a vascular suture of the venotomy site on the anterior wall was performed with 7/0 polypropylene. Clamps were removed, and satisfactory blood flow through the IJV was confirmed (Fig. 5).
The postoperative course was uneventful. Sutures were removed on day 12 after surgery, after which the patient was discharged and evacuated to the next stage of medical care. The following therapy was administered: apixaban 5 mg twice daily; ceftriaxone 1.0 g twice daily intramuscularly; analgesics.
According to ultrasonography findings, on the first day and on day 12 after surgery, the internal jugular vein (IJV) was patent, with no signs of thrombosis or restenosis.

Photograph taken by the authors
Fig. 1. Fragment wound of the left shoulder: 1 — the entrance wound is located on the posterior surface of the left shoulder
Images obtained by the authors
Fig. 2. Neck radiography: 1 — lateral neck radiography: metallic foreign body (fragment) in the left neck tissues; 2 — anteroposterior neck radiography: metallic foreign body (fragment) in the left neck tissues
Images obtained by the authors
Fig. 3. Left neck ultrasound: 1 — floating thrombus in the lumen of the internal jugular vein; 2 — metallic foreign body (fragment) penetrating the lumen of the internal jugular vein; 3 — site of attachment of the floating thrombus to the metallic foreign body (fragment)

Photograph taken by the authors
Fig. 4. Foreign metallic body (fragment) and thrombotic material removed from the internal jugular vein
Photograph taken by the authors
Fig. 5. Final result of the operation: 1 — closure of the venotomy site on the anterior wall of the internal jugular vein; 2 — internal jugular vein proximal to the site of reconstruction
DISCUSSION
The current literature lacks sufficient studies on the surgical management of neck injuries in servicemen during combat operations. Anipchenko et al. described a case of gunshot wound to the neck [9]. The fragment did not damage blood vessels, being localized paraesophageally in the Killian’s triangle region. Subsequently, an abscess developed, requiring surgical intervention. Successful open surgery was performed to remove the foreign body and fragment. The postoperative course was uneventful [9]. This case highlights that foreign bodies (fragments) in deep neck tissues, even without causing bleeding, should be removed due to high risks of infectious complications, abscess formation, and mediastinitis.
Dadayan et al. presented a case of foreign body removal from the neck after fragment wound [10]. However, the fragment did not damage the neurovascular bundle. According to ultrasound, it was localized between the jugular vein and common carotid artery. The fragment was removed via open surgery under ultrasound guidance. The procedure was completed without complications [10]. The authors emphasized the importance of such operations due to risks of neurovascular bundle injury from foreign body migration.
Muminjonova et al. [7] reported a case of fragment wound to the neck with injury to carotid arteries, resulting in pseudoaneurysm formation. Aneurysm resection with subsequent prosthetic grafting was performed. This approach prevented potential aneurysm rupture-related bleeding and wound infection [7].
The clinical case presented in this article is the first report of a military-field surgical intervention describing surgical management of a neck fragment wound with fragment invasion into the IJV and floating thrombus formation. The technological complexity was due to the IJV wall defect being located on its posterior surface, preventing adequate thrombectomy and subsequent repair. Thus, it was decided to perform anterior IJV venotomy, open thrombectomy, followed by posterior wall repair and venotomy closure. A 7/0 polypropylene suture was used for vascular repair to minimize vein incorporation and prevent residual restenosis. In our opinion, IJV ligation without reconstruction could acutely impair cerebral venous outflow, leading to venous congestion and potential cerebral edema.
Thus, the implemented surgical strategy has proven successful and allowed optimal treatment outcomes to be achieved.
CONCLUSION
The presented case demonstrates previously unpublished data on a variant of fragment injury to the internal jugular vein. The proposed surgical technique has proven to be effective and safe. Its implementation prevented the development of distal embolism, wound infection, and bleeding.
1 Decree No. 855 of the Government of the Russian Federation of 29.07.1998 “On Measures to Implement the Federal Law ‘On Compulsory State Insurance of Life and Health of Military Personnel, Citizens Called up for Military Training, Privates and Commanders of Internal Affairs Agencies of the Russian Federation, and Employees of Federal Tax Police Bodies’”.
References
1. Oppel VA. Report of the Head of the Medical Unit of the Red Cross at the Caucasian Army, Professor V.A. Oppel. Petrograd: Gov. print; 1915 (In Russ.).
2. Pchelina IV. Surgical care for the wounded with damage to the main vessels in wartime (on the 80th anniversary of the military operations at Lake Khasan). Bulletin of the A.N. Bakulev Scientific Center for Cardiovascular Surgery, Russian Academy of Medical Sciences. Cardiovascular diseases. 2018;19(S6):281 (In Russ.). EDN: YNTCSL
3. Akhutin MN. Surgical work during the battles at Lake Khasan. Moscow: Medgiz; 1939 (In Russ.).
4. Petrovsky BV. Surgical treatment of vascular injuries. Moscow: Academy of Medical Sciences of the USSR’ printing house; 1949 (In Russ.).
5. Pirogov NI. Principles of General Military Field Surgery. Collected Works. Volume 8. Moscow: Medgiz; 1961 (In Russ.).
6. Koroleva KYu, Savchenko IF, Borisov DN, Gaidakov GA. Medical and statistical characteristics of combat otolaryngological pathology. Bulletin of the Russian Military Medical Academy. 2020;39(S4):301–4 (In Russ.). EDN: KMXQUS
7. Muminzhonova MM, Antonov GI, Chmutin GE, Miklashevich ER, Manukovskiy VA, Chmutin EG, et al. Gunshot wounds of the extracranial division of the carotid basin with the formation of false aneurism. Clinical observation staged treatment and literature review. Bulletin of Neurology, Psychiatry and Neurosurgery. 2025;4:480–92 (In Russ.). https://doi.org/10.33920/med-01-2504-07
8. Kharchenko OYu, Kazantsev AN, Alekseev OV, Makhmudov RM, Kholmatov VN, Tenishev RR. Resection of false posttraumatic aneurysm of the axillary artery within a separate medical airmobile detachment in special military operation zone. Pirogov Russian Journal of Surgery. 2025;6:122–7 (In Russ.). https://doi.org/10.17116/hirurgia2025061122
9. Anipchenko SN, Arkhangelsky DA, Kuznetsov SA, et al. Gunshot wound of the neck with a fragment localized in close proximity to the initial part of the esophagus with development of paraesophageal abscess. Surgical tactics. Surgical tactics. Surgeon. 2024;3–4:60–9 (In Russ.). https://doi.org/10.33920/med-15-2402-06
10. Dadayan AR, Belik BM, Tenchurin RS, Bolotskov AS. Ultrasound-Guided Removal of Deep-Lying Foreign Bodies of the Soft Neck Tissue in a Patient with a Shrapnel Wound. Journal of Experimental and Clinical Surgery. 2024;17(2):66– 71 (In Russ.). https://doi.org/10.18499/2070-478X-2024-17-2-66-71
About the Authors
D. S. VasilievRussian Federation
Dmitry S. Vasiliev
A. N. Kazantsev
Russian Federation
Anton N. Kazantsev - Cand. Sci. (Med.)
V. V. Kolesnikov
Russian Federation
Vladimir V. Kolesnikov
R. P. Yakimavichus
Russian Federation
Roman P. Yakimavichus
A. G. Shishkin
Russian Federation
Alexander G. Shishkin
Zh. M. Belyai
Russian Federation
Zhanna M. Belyai
R. R. Tenishev
Russian Federation
Ramil R. Tenishev
V. V. Kholmatov
Russian Federation
Vadim V. Kholmatov
Supplementary files
Review
For citations:
Vasiliev D.S., Kazantsev A.N., Kolesnikov V.V., Yakimavichus R.P., Shishkin A.G., Belyai Zh.M., Tenishev R.R., Kholmatov V.V. Removal of a metal fragment and floating thrombus from the internal jugular vein of a serviceman in a field hospital. Extreme Medicine. 2025;27(4):500-504. https://doi.org/10.47183/mes.2025-349

















