Scroll to:
Pathobiochemical aspects of divers barodentalgia
https://doi.org/10.47183/mes.2024-26-3-65-70
Abstract
Introduction. During their descent under water, divers may suffer from acute toothache attacks (barodentalgia), creating an emergency that leads to the termination of diving descent. Barodentalgia can be caused by hypoxic process in the pulp of filled teeth under increased intrapulpal pressure.
Objective. To reveal the peculiarities of hypoxic processes in the pulp of filled teeth under hyperbaric exposure basing on oximetry and fluorescence change parameters.
Мaterials and methods. The study involved 34 male divers who underwent a dental examination at the first stage to select individuals for the second stage of the experiment. 24 subjects were selected for the second stage and evaluated for oximetric (mixed blood saturation) and fluorescent (reduced coenzyme NADH, oxidized coenzyme FAD, fluorescent oxygen consumption index — FOCI) indices of filled teeth. The evaluation was performed by optical tissue oximetry (OTO) and laser-induced fluorescence (LIF) methods before and after immersion in a barocamera at pressure of 0.4 MPa while breathing air.
Results. Following exposure to increased pressure of the gas medium as compared to the initial values in the filled teeth, the following phenomena were observed: decrease in pulp saturation by 33.7% (p<0.05); increase in NADH by 14.4%; decrease in FAD by 22.9%; increase in FOD by 73.4% (p<0.05).
Conclusions. The revealed changes in the indicators of mixed blood saturation, NADH, FAD and FOCI confirm the presence of hypoxic process in the pulp of filled teeth under hyperbaric exposure.
For citations:
Klenkov I.R., Krivonos A.S., Grashin R.A., Pototskaya A.V., Zheleznyak V.A., Maday I.S. Pathobiochemical aspects of divers barodentalgia. Extreme Medicine. 2024;26(3):65-70. https://doi.org/10.47183/mes.2024-26-3-65-70
INTRODUCTION
When diving under water, a person is affected by numerous factors of increased environmental pressure (the value of the total pressure and its variations, increased partial pressure of gases, high density of the gas mixture, frequency and duration of period under pressure, increased heat capacity and thermal conductivity of water, mechanical impact of equipment, etc.), forming specific conditions of diving labor and causing changes in the state of the human body some of which may be pathological [1].
Such pathological manifestations can significantly reduce professional efficiency of a diver and create an emergency situation, which inevitably entails reduction of professional longevity. One such pathological condition is barodentalgia, a syndrome arising under conditions of altered environmental pressure characterized by attacks of acute or aching toothache, as well as painful sensations in the dental row area [2].
According to research [2], one of the risk factors for barodentalgia in divers is the presence of filled teeth. In the pathogenesis of barodentalgia, an important role may be played by the hypoxic process, which develops in the pulp chamber of filled teeth as a result of impaired microcirculation. Hypoxic processes occur as a result of peripheral pulp vessels narrowing under the impact of increased environmental pressure and reduction of the pulp chamber in volume due to the formation of replacement dentin — a plastic process of the pulp that occurs in response to the consequence of damage to the hard tissues of the tooth (carious lesion).
Various methods are currently used to perform a quantitative assessment of metabolic processes occurring in human tissues — in particular, in the dental pulp [3–4]. In the present context, the most accessible techniques include optical tissue oximetry (OTO) and laser-induced fluorescence (LIF) [5]. These techniques allow to assess not only tissue parameters in general, but also changes in cellular metabolism characteristic of the hypoxic process in the dental pulp.
The purpose of the study is to identify the peculiarities of hypoxic processes in the pulp of intact and filled teeth under hyperbaric exposure on the basis of changes in the oximetry and fluorescence parameters.
МАТERIALS AND METHODS
Under the auspices of the Military Medical Academy, we conducted a study with the participation of the Northern Fleet divers (n = 34), who were selected for the presence of barodentalgia in the anamnesis revealed via questioning using a questionnaire developed by us, as well as those referred for health reasons. The age of the experimental subjects ranged from 24 to 47 years. All subjects were male. The study was carried out in two stages.
At the first stage of the study, 34 individuals were selected based on oral examination data and analysis of cone beam computed tomograms (hereinafter referred to as CBCTs). The main selection criterion for participation in the study was the presence of a pair of symmetrical teeth (one morphofunctional group) in which one tooth was affected by barodentalgia and the second tooth was intact. 24 testers were selected for the second stage.
At the second stage of the study, we evaluated oximetric and fluorescent indices of intact and filled teeth of 24 subjects by the method of oxidative metabolism diagnostics using the LASMA-D apparatus (Russia) before and after immersion in the flow-decompression chamber KVD-1600 (Russia) for a duration of 125 minutes at a pressure of 0.4 MPa under a special decompression mode with air breathing.
The following parameters were measured: mixed blood (arterial and venous) saturation using the technique of optical tissue oximetry (OTO), fluorescence emission amplitude of reduced coenzyme NADH and oxidized coenzyme FAD using the technique of laser-induced fluorescence (LIF).
Based on the fluorescence spectra obtained under excitation by external radiation, we calculated the fluorescence oxygen consumption index (FOCI), which reflects the redox potential in intracellular mitochondria, according to the formula [5]:
 (1)
(1)
where FOCI — fluorescent indicator of oxygen consumption; ANADH — amplitude of fluorescence emission of the reduced nicotinamide adenine dinucleotide coenzyme; AFAD — amplitude of fluorescence emission of oxidized flavoproteins.
Mathematical data processing was carried out on a personal computer using the software package “StatSoft STATISTICA 10”. Quantitative data were checked for compliance with the theoretical Gauss-Laplace distribution law using the Shapiro-Wilk criterion. The groups were compared using the Mann-Whitney U-criterion.
STUDY RESULTS
During the collection of anamnesis data, the tooth subjected to barodentalgia was identified. It was also determined that barodentalgia occurred in filled teeth with clinically complete fillings, in carious teeth with different localization of the carious process and in teeth with caries recurrence. Based on the results of the dental examination, 24 individuals were selected, each having a pair of symmetrical teeth (of the same morphofunctional group), in which one tooth was barodontalgic while the other was intact. Filled teeth with clinically complete fillings and without signs of caries recurrence, in which the filling material was located within the peri-pulpal dentin, were selected for the study.
The incidence of filled teeth was significantly higher in the masseter group of the jaws than in the anterior group. Figure 1 shows an example of a CBCT of an experimental subject who met the selection criteria for participation in the study.
At the second stage, to evaluate oximetric and fluorescent parameters, we examined the molar groups of teeth of the upper and lower jaws due to the high frequency of occurrence (p < 0.05) of filled teeth in this localization compared to other groups.
The results of oximetric and fluorescence diagnostics are presented in Table 1.
Figure 2 shows the results of OTO. Following exposure to elevated pressure, the mixed blood saturation level in intact teeth increased by 19.4%, while in filled teeth it decreased by 33.7% compared to baseline, which is a statistically significant change (p < 0.05).
While a decrease in the mixed blood saturation level in the filled teeth following hyperbaric exposure indicates the presence of a hypoxic process in the pulp, our tasks were, firstly, to identify the cause of this process, and secondly, to determine the changing vector in the metabolic processes of intact and sealed teeth at the tissue level, forming the basis for an extended LIF-used diagnostics of pulp.
The results of the LIF are presented in the table. The initial value of the fluorescence emission amplitude of the reduced NADH coenzyme in intact teeth was 15.5% higher than after hyperbaric exposure. The initial NADH level in the filled teeth turned out to be 14.4% lower on average than after hyperbaric exposure. The data of the NADH indicator are not statistically strong.
The initial values of the fluorescence emission amplitude of the oxidized coenzyme FAD in intact teeth turned out to be significantly higher than those after exposure to increased pressure by an average of 34.5%. The initial values of the same indicator for the filled teeth were higher than after exposure to increased pressure by an average of 22.9%. The data of the FAD indicator are not statistically expressed.
The results of calculating the fluorescent indicator of oxygen consumption are shown in Figure 3. Under normobaric conditions, the FPC in intact teeth was 23.5% lower than after hyperbaric exposure. The initial values of FPC in the filled teeth were statistically significantly lower than after hyperbaric exposure by an average of 73.4% (p < 0.05).
Thus, changes in saturation and FPC indicators reveal a hypoxic process in sealed teeth that occur under conditions of increased gas pressure, whereas in intact teeth a change in this indicator is a sign of a slight decrease in the activity of metabolic processes.
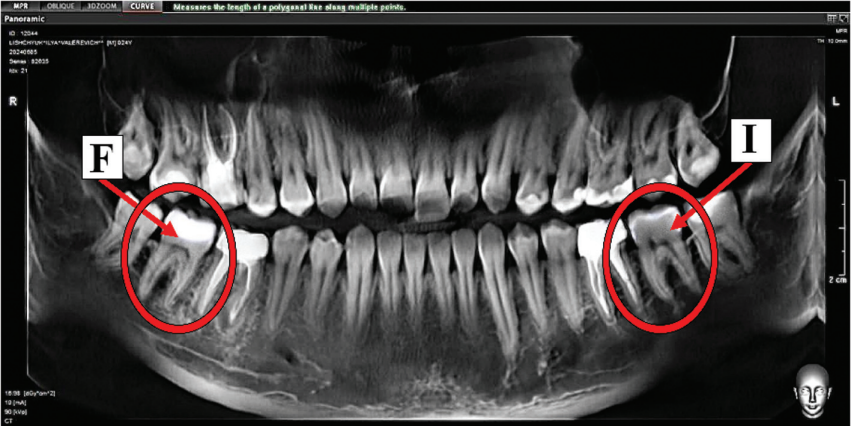
The figure was prepared by the authors using their own data
Fig. 1. Panoramic section of the cone-beam computed tomogram of diver V. (P is a filled tooth, and E is an intact tooth)
Table 1. Oximetric and fluorescence diagnostic results
|
Indicator |
Tooth condition |
Descent period |
Me [Q25;Q75] |
Degree of change, % |
|
Oximetric indicators (GRT) |
||||
|
Saturation |
intact |
before hyperbaric exposure |
38.1[ 28.9;49.3] |
19.40 |
|
after hyperbaric exposure |
45.5[ 38.5;56.6] |
|||
|
filled |
before hyperbaric exposure |
19.6[ 11.9;35.3] |
–33.70* |
|
|
after hyperbaric exposure |
13.0[ 5.7;23.0] |
|||
|
Fluorescent indicators (LIF) |
||||
|
NADH |
intact |
before hyperbaric exposure |
1.16[ 0.87;1.22] |
–15.50 |
|
after hyperbaric exposure |
0.98[ 0.82;1.16] |
|||
|
filled |
before hyperbaric exposure |
1.11[ 0.92;1.20] |
14.40 |
|
|
after hyperbaric exposure |
1.27[ 1.17;1.38] |
|||
|
FAD |
intact |
before hyperbaric exposure |
1.13[ 0.88;1.28] |
–34.50 |
|
after hyperbaric exposure |
0.74[ 0.62;0.98] |
|||
|
filled |
before hyperbaric exposure |
1.18[ 0.965;1.31] |
–22.90 |
|
|
after hyperbaric exposure |
0.91[ 0.685;1.16] |
|||
|
FOCI |
intact |
before hyperbaric exposure |
1.02[ 0.83;1.42] |
23.50 |
|
after hyperbaric exposure |
1.26[ 0.92;1.43] |
|||
|
filled |
before hyperbaric exposure |
0.94[ 0.77;1.23] |
73.40* |
|
|
after hyperbaric exposure |
1.63[ 1.33;1.84] |
|||
The table was prepared by the authors using their own data
Note: * — p < 0.05
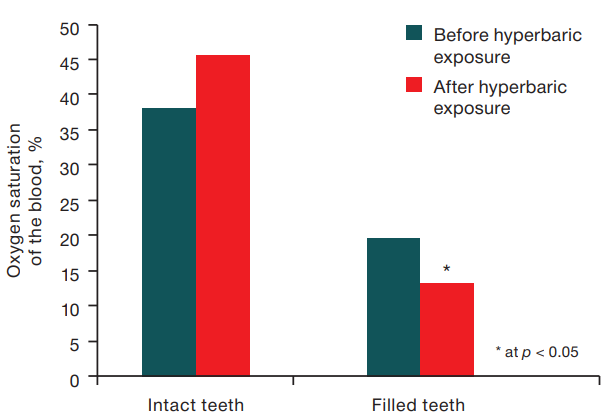
The figure was prepared by the authors using their own data
Fig. 2. Change in the oximetric indices of mixed blood saturation (р < 0.05)
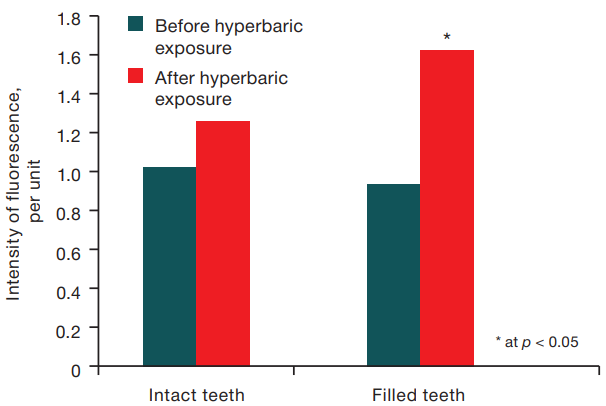
The figure is prepared by the authors using their own data
Fig. 3. Change in fluorescence index of oxygen consumption (р < 0.05)
DISCUSSION OF THE RESULTS
The calculated FPC indicator, which is based on determining the activity of intracellular mitochondria, indirectly reflects the level of oxygen metabolism in cells; however, in our study this indicator turned out to be very informative, since it allowed us to determine the presence of a hypoxic process in the pulp of filled teeth.
According to C.M. Math et al. (2017), centralization of blood flow under conditions of increased environmental pressure is followed by the development of a compensatory adaptive reaction in the form of narrowing of peripheral vessels against the background of a systemic increase in blood pressure [2]. In the pulp of the filled teeth, which are reduced in volume due to the formation of substitutive (tertiary) dentin, vasoconstriction leads to a significant decrease in microcirculation and perfusion.
With insufficient perfusion of the filled tooth tissues, an energy deficit occurs due to the participation of oxygen as a substrate of cytochrome oxidase in aerobic energy formation reactions. Lack of oxygen leads to a change in the enzyme complexes activity of the respiratory chain and a decrease in the level of adenosine triphosphate (ATP). This has a detrimental effect on energy-dependent cellular reactions, e.g., the formation of membrane potential, ion transport, electrogenic cell function, etc. [6–7].
A partial blockade of the respiratory chain also leads rapidly to an excessive concentration of reduced coenzymes such as NADH and FADH2, which spontaneously dissociate with the release of protons to increase intramitochondrial hypoxia. This stage is characterized by an even greater slowdown in the oxidation of substrates in the tricarboxylic acid cycle and oxidative decarboxylation of pyruvic acid, increasing the accumulation of lactic acid (lactate) due to glycolysis under these conditions becoming the main energy process in the pulp cells of sealed teeth, while a high level of lactate contributes to an increase in the concentration of pyruvic acid and/or NADH [8–9].
The hypoxic process causing the development of an energy deficit of pulp cells triggers the release of biologically active substances such as bradykinin, serotonin, neuroactive peptides, etc., which, acting on the microvessels of the pulp, lead to vasodilation and increased vascular permeability, which entails an increase in intrapulpal pressure.
Why does barodentalgia occur? It may be caused by an increase in intrapulpal pressure, leading to irritation of nerve endings, since the pulp chamber of the filled tooth is reduced in volume due to the formed replacement dentin [10–11] and constant pressure of the filling material on the tooth pulp [12–13]. In intact teeth, the volume of the pulp chamber is of normal size, which does not cause an increase in intrapulpal pressure. At the stage of energy deficiency in the filled teeth, it is also worth noting the increase in the concentration of lactic acid in the intercellular space that contains a large number of nerve endings, which may in all likelihood exacerbate the development of barodentalgia [14]. Biologically active substances such as bradykinin, serotonin, etc. can additionally increase the intensity of barodentalgia [15].
CONCLUSIONS
- Following exposure to altered environmental pressure, there was a statistically significant decrease in mixed blood saturation in pulp vessels by an average of 33.7%, an increase in the fluorescence intensity of reduced NADH coenzymes by 14.4%, and a decrease in the fluorescence intensity of oxidized FAD coenzymes by 22.9% as compared with intact teeth.
- The calculated index of the FPC of the filled teeth after exposure to increased environmental pressure significantly increased by 73.4% as compared with the identical index in intact teeth. The above changes in the studied indicators confirm the fact of the presence of a hypoxic process in the pulp of sealed teeth in divers under conditions of increased environmental pressure as compared with intact teeth. The exact mechanism by which a number of pathophysiological and biochemical changes trigger the development of barodentalgia due to the hypoxic process requires further research.
References
1. Zverev DP, Klenkov IR, Myasnikov AA, Shitov AYu, Fisun AV, Starkov AV, et al. The human body’s resistance to the action of high partial pressures of nitrogen and methodological aspects of its assessment. Marine medicine. 2020;(4):44–53 (In Russ.). https://doi.org/10.22328/2413-5747-2020-6-4-44-53
2. Pototskaya AV, Krivonos AS, Polikarpochkin AN, Klenkov IR, Poplaukhin TS, Klenkova DA. The effect of increased pressure of the gaseous medium on the microcirculation of teeth. Doctor. 2023;(3):66–9 (In Russ.). https://doi.org/10.29296/25877305-2023-03-14
3. Loginova NK, Ermolyev SN, Shiryaev AP Reactive changes in capillary blood flow in dental pulp in dental caries and the development of pulpitis. Endodontics Today. 2011;(2):20–2 (In Russ.). EDN: OFYWBD
4. Loginova NK, Troitskaya TV. Laser Doppler flowmetry of tooth pulp (literature review) (Part I). Institute of Dentistry. 2007;(1):110–1 (In Russ.). EDN: MWGUPJ
5. Moskvin SV, Antipov EV, Zarubina EG, Ryazanova EA. Efficiency of oxygen metabolism after the application of laserophoresis of various gels based on hyaluronic acid. Bulletin of Aesthetic Medicine. 2011;(3):48–55 (In Russ.). EDN: RABTEX
6. Skvortsov VV, Skvortsova EM, Bangarov RYu. Lactate acidosis in the practice of an anesthesiologist-resuscitator. Bulletin of Anesthesiology and Intensive Care. 2020;(3):95–100 (In Russ.). https://doi.org/10.21292/2078-5658-2020-17-3-95-100
7. Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014; 371(24):2309–19. https://doi.org/10.1056/NEJMra1309483
8. Robergs RA, Ghiasvand F, Parker D. Biochemistry of exerciseinduced metabolic acidosis. Am J Physiol Regul Integr Comp Physiol. 2004;287(3):R502–16. https://doi.org/10.1152/ajpregu.00114.2004
9. Windpessl M, Wallner M. Lactic acidosis. N Engl J Med. 2015;372(11):1077. https://doi.org/10.1056/NEJMc1500327
10. Choung HW, Lee DS, Lee JH, Shon WJ, Lee JH, Ku Y, Park JC. Tertiary Dentin Formation after Indirect Pulp Capping Using Protein CPNE7. J Dent Res. 2016; 95(8):906–12. https://doi.org/10.1177/0022034516639919
11. Lee M, Lee YS, Shon WJ, Park JC. Physiologic dentin regeneration: its past, present, and future perspectives. Front Physiol. 2023;14:1313927. https://doi.org/10.3389/fphys.2023.1313927
12. Kamalak H, Kamalak A, Taghizadehghalehjoughi A. Cytotoxic effects of new-generation bulk-fill composites on human dental pulp stem cells. Cell Mol Biol (Noisy-le-grand). 2018;64(3):62–71. https://doi.org/10.14715/cmb/2018.64.3.11
13. Costa CA, Giro EM, do Nascimento AB, Teixeira HM, Hebling J. Short-term evaluation of the pulpo-dentin complex response to a resin-modified glass-ionomer cement and a bonding agent applied in deep cavities. Dent Mater. 2003;19(8):739–46. https://doi.org/10.1016/s0109-5641(03)00021-6
14. Jha MK, Song GJ, Lee MG, Jeoung NH, Go Y, Harris RA, Park DH, Kook H, Lee IK, Suk K. Metabolic Connection of Inflammatory Pain: Pivotal Role of a Pyruvate Dehydrogenase Kinase-Pyruvate Dehydrogenase-Lactic Acid Axis. J Neurosci. 2015;35(42):14353–69. https://doi.org/10.1523/JNEUROSCI.1910-15.2015
15. McHugh JM, McHugh WB. Pain: neuroanatomy, chemical mediators, and clinical implications. AACN Clin Issues. 2000;11(2):168–78. https://doi.org/10.1097/00044067-200005000-00003
About the Authors
I. R. KlenkovRussian Federation
Saint-Petersburg
A. S. Krivonos
Russian Federation
Saint-Petersburg
R. A. Grashin
Russian Federation
Saint-Petersburg
A. V. Pototskaya
Russian Federation
Saint-Petersburg
V. A. Zheleznyak
Russian Federation
Saint-Petersburg
I. S. Maday
Russian Federation
Saint-Petersburg
Supplementary files
Review
For citations:
Klenkov I.R., Krivonos A.S., Grashin R.A., Pototskaya A.V., Zheleznyak V.A., Maday I.S. Pathobiochemical aspects of divers barodentalgia. Extreme Medicine. 2024;26(3):65-70. https://doi.org/10.47183/mes.2024-26-3-65-70
















