Scroll to:
Injuries and damage to large joints in underage athletes. Therapy with platelet-rich plasma. A clinical case
https://doi.org/10.47183/mes.2025-323
Abstract
Introduction. Approximately 46% of large joint injuries involve damage to the knee joint, among which anterior cruciate ligament (ACL) injuries account for about 15–24% in children and adolescents. In order to reduce the likelihood of long-term complications after injuries in underage professional athletes, shorten the rehabilitation period, and enable a quicker return to elite sports, innovative regenerative medicine technologies should be implemented into clinical practice, including the use of platelet-rich plasma (PRP). In comparison with other conservative treatment methods, PRP offers several advantages. Being an orthobiological agent, PRP is a biological substance derived from the patient’s own body, promoting accelerated regeneration with minimal risk of side effects. When performed correctly, this procedure shows minimal invasiveness and does not lead to complications. Although PRP therapy is widely used in treating diseases and injuries of large joints in adult patients, the application of this therapeutic method in underage athletes has not been sufficiently studied, which is the focus of this study.
Case report. We present a clinical case of a professional athlete with a knee joint injury, assessing the functional and clinical outcomes of PRP therapy. Two standardized methods for PRP application are demonstrated, highlighting the advantages of a closed-loop PRP preparation system. These include minimized exposure to the external environment, mitigating potential risks of infection, and reduced consumption of materials, enhancing cost-effectiveness. The described clinical case of an ACL injury in a junior athlete, with complete functional and structural recovery (as confirmed by magnetic resonance imaging, MRI), demonstrated the efficacy, safety, and good tolerability of PRP therapy. Positive outcomes were observed both clinically (regression of pain assessed via the visual analog scale, restoration of joint function, and positive dynamics in provocative tests such as the Lachman test and anterior drawer test) and through MRI data.
Conclusions. The use of PRP therapy for ACL injuries in underage professional athletes represents a promising therapeutic approach in orthopedics and sports medicine, utilizing regenerative medicine technologies. The closed-loop system for PRP preparation offers several advantages over open-loop systems, including cost-effectiveness due to minimized consumption of medical supplies. The safety of the method is ensured provided that the procedural requirements are met (asepsis, antisepsis, ultrasound guidance, etc.); the high sensitivity of MRI in tracking the dynamics of ACL injuries is confirmed.
Keywords
For citations:
Zyabkin I.V., Pankratov I.V., Kovalkova A.M., Khizhnikova V.V., Zavaleva E.V., Mukhortykh V.A. Injuries and damage to large joints in underage athletes. Therapy with platelet-rich plasma. A clinical case. Extreme Medicine. 2025;27(4):542-549. https://doi.org/10.47183/mes.2025-323
INTRODUCTION
The development of physical culture and sports, including youth sports, is a priority direction of Russian state policy.1 2 According to the list of instructions of the President of Russia,3 the Federal Medical and Biological Agency (FMBA) serves as the lead organization for medical support and biomedical supervision of athletes in Russian national teams. This role, combined with the country’s strategic national priorities in scientific and technological development, drives the adoption of innovative technologies in sports medicine.4
In Russia, approximately 24.3 million children regularly engage in physical culture, with 3.2 million training in sports centers. Elite sports involve about 17,000 children. Sports-related injuries account for about 35.8% of all injuries among children (aged 5–17) [1]. Knee injuries dominate (approximately 46% of all major joint injuries), with anterior cruciate ligament (ACL) injuries remaining highly prevalent among professional athletes, children, and adolescents. These are severe conditions, comprising 15–24% of such injuries, while meniscus trauma occurs at a rate of 5.1 per 100,000 juniors [2][3]. Upper limb injuries (shoulder, elbow joints) are common among athletes (including children) involved in overhead activities. In 75% of cases, these injuries result in temporary exclusion from sports [4], yet only 5% require surgical intervention [5].
The development of physical culture and sports in Russia has led to a growing number of professional athletes, increasing the incidence of sports-related injuries. This trend necessitates the adoption of novel therapeutic approaches, including regenerative medicine technologies such as the use of platelet-rich plasma (PRP).
PRP, as an orthobiological agent and a biological substance derived from the patient’s own body, accelerates recovery and promotes regeneration, alleviates pain, and shortens the rehabilitation period. This is particularly critical in elite sports [6][7]. Moreover, when performed according to guidelines, PRP therapy is a minimally invasive technique with a low complication rate [8]. While numerous publications address the use of PRP for joint diseases in adults with osteoarthritis and in older professional athletes [9][10], studies evaluating the efficacy of PRP in underage athletes with injuries to large joints remain insufficient.
This work presents a clinical case of a professional athlete with a knee joint injury, assessing the functional and clinical outcomes of PRP therapy.
Preparation of Platelet-Rich Plasma (PRP)
Injuries and damage to various segments of the limbs are an unfortunate but integral part of elite sports. PRP has been successfully applied in such conditions as tennis elbow, golfers elbow, Achilles tendon injuries and plantar fasciitis, rotator cuff syndrome, adductor enthesopathy, jumpers knee, and runners knee [11].
PRP is human blood plasma with a concentration of platelets exceeding physiological levels. Platelets are anucleate cytoplasmic bodies formed through the fragmentation of megakaryocyte precursors. They circulate in the blood, expressing glycoproteins on their cell membranes, playing a key role in hemostasis and wound healing through the formation of fibrin clots [12].
A number of studies have shown that platelet counts in healthy individuals change throughout life. The normal platelet count for adults of both sexes ranges (150–400)×109/L. In children, platelet levels vary with age during growth and development. For example, in a one-month-old child, the platelet count is (208–352)×109/L, reaching about (198–340)×109/L5 by age 11.
PRP is obtained by separating platelets from other blood components through the collection of a specific volume of the patient’s blood followed by centrifugation. This process yields blood plasma with a high platelet concentration (exceeding the physiological baseline by 3–10 times). The final platelet concentration may vary depending on the system used [13][14].
Currently, a substantial number of scientific studies are dedicated to randomized clinical trials on the use of PRP therapy for injuries and disorders of the musculoskeletal system [15, 16], including in professional athletes. However, Russia lacks a unified approved methodology for injections of PRP. To standardize the approach to PRP application for injuries and damage to large joints in junior athletes, two methods have been approved at the Federal Scientific and Clinical Center for Children and Adolescents: open and closed (Fig. 1).
When processed using a closed-loop system, platelets are not exposed to the external environment after blood collection. This system involves the use of a commercial kit, primarily in combination with additional centrifugation.
There are numerous (over 40) protocols and commercial systems for producing PRP; the relevant data are presented in Table.
The study by Jildeh et al. present a comparative analysis of PRP preparation methods using commercial systems. Technical specifications, cost, processing time, and centrifugation parameters of various commercially available PRP devices differ significantly. The physician independently determines the characteristics that best align with their PRP requirements [17].
CLINICAL CASE DESCRIPTION
Patient A, 16 years old (born 2007), a professional beach volleyball athlete, was under observation at the Traumatology Department of the Federal Scientific and Clinical Center for Children and Adolescents with the following diagnosis: S83.7 Injury of multiple structures of the knee joint. Partial tear of the anterior cruciate ligament (ACL) of the left knee joint. W09.3 Fall involving sports ground equipment during sports activities and competitions.
Medical History. The patient is the first child from a physiological pregnancy and spontaneous delivery. Birth weight was 3450 g, length 52 cm, Apgar score 8–9. Breastfeeding continued until 10 months. Psychomotor development during the first year was age-appropriate. Past infectious diseases: ARVI, chickenpox. Preventive vaccinations were administered according to the national immunization schedule. No prior surgical interventions.
History of Present Illness. In March 2025, during training, the patient sustained a left knee injury due to a fall. Given the trauma and severe pain, magnetic resonance imaging (MRI) of the injured joint was performed outpatient at the local clinic. The MRI findings indicated an isolated ACL injury of the left knee joint (Fig. 2A). Two days post-injury, the patient was examined by a trauma orthopedist at the Federal Scientific and Clinical Center for Children and Adolescents.
Status Localis. Moderately pronounced edema in the left knee joint; positive patellar ballottement sign; flexion limited to 90° due to pain. Provocative tests (Lachman test, anterior drawer test) could not be performed at this stage due to severe pain. Pain intensity assessed via the Visual Analog Scale (VAS) (0 = no pain, 10 = worst pain) was 5 points.
Based on the history, complaints, physical examination, and diagnostic results, the final diagnosis was “Isolated injury of the anterior cruciate ligament of the left knee joint.”
Management and Treatment Strategy. To reduce pain and stimulate regeneration of damaged tissues, a conservative treatment strategy was selected. This included immobilization of the knee joint (tutor for 2 weeks), troxerutin gel (for 2 weeks) cold therapy (3 days) for local treatment, of a hinged brace with gradual increase in flexion angle by 15–30° every 3 days, exclusion of running and jumping, and a course of PRP therapy (3 injections at 7-day intervals). After six months of the PRP therapy course, a follow-up MRI was conducted.
PRP Therapy. In accordance with the protocol developed and implemented at the Federal Scientific and Clinical Center for Children and Adolescents for candidate selection for PRP therapy, the patient was evaluated using inclusion criteria before initiating the PRP course. This included assessment of complete blood count (CBC) and inflammatory markers (C-reactive protein, CRP) to promptly identify signs of systemic inflammation or other contraindications. Additionally, prior to each injection, CBC was repeated to rule out potential contraindications (e.g., acute inflammatory processes, thrombocytopenia). Given normal laboratory values and no deviations from other inclusion criteria, the athlete received a course of PRP therapy consisting of three injections at seven-day intervals.
For platelet-rich plasma preparation, a closed-loop method using a dual-syringe system was selected: 15 mL of whole blood was collected from the medial cubital vein into Arthrex tubes and centrifuged at 1500 rpm for 5 min using a Rotofix 32A centrifuge. After blood component separation, the formed platelet-rich plasma layer (approximately 5.0 mL) was transferred from the outer syringe to the inner syringe. A portion of the prepared material (approximately 1.0 mL) was sent to a clinical diagnostic laboratory for platelet concentration measurement, which confirmed a twofold increase in platelet count compared to baseline. PRP injections were administered percutaneously under ultrasound guidance. The procedure was performed under aseptic conditions after skin antisepsis, with the patient in a supine position and the knee flexed at 90°. The injection was delivered into the knee joint cavity via a lateral approach. The patient tolerated PRP therapy satisfactorily, with no adverse reactions reported.
Therapy Results. After the completed course of PRP therapy, the patient noted improvement in knee joint function manifested in reduced pain syndrome (VAS – 3 points), improved flexion function, and decreased discomfort phenomena in the left knee joint during physical exercises.
The follow-up examination after six weeks showed a complete regression of the edema of the knee joint area, a full restoration of the joint flexion, and the absence of pain syndrome (VAS – 1 point). Slight limping was noted when leaning on the injured limb. Provocative tests (Lachman test and anterior drawer test) were questionable; however, no signs of pronounced instability were detected. Importantly for the athlete, gradual return to previous sports load was noted, including running and cycling. Five months after the injury, the patient was able to resume gym training (leg press with 120 kg weight).
The follow-up examination six months after the injury showed the ability of the patient to walk independently and confidently, without limping. No edema in the left knee joint area was present; the patella was in the midline. Ballottement sign was negative, Lachman and anterior drawer tests were negative, symmetrical on both sides. No subjective or objective signs of knee joint instability were detected, VAS was 0 points. Therefore, according to control MRI data, restoration of the anterior cruciate ligament structure was confirmed (Fig. 2B).
Thus, this clinical case demonstrates the efficacy, safety, and good tolerability of PRP application for ACL injury in an underage professional athlete. Positive outcomes were observed both clinically — manifested as regression of pain assessed via VAS, restoration of joint function, and positive dynamics in provocative tests (Lachman test and anterior drawer test) — and through MRI data showing restoration of the anatomical integrity of the ligament. This highlights the importance of an individualized approach to treatment strategies for patients, particularly athletes with injuries and damage to large joints. The results align with current literature data, indicating the promise of therapeutic approaches in orthopedics and sports medicine utilizing regenerative medicine technologies.
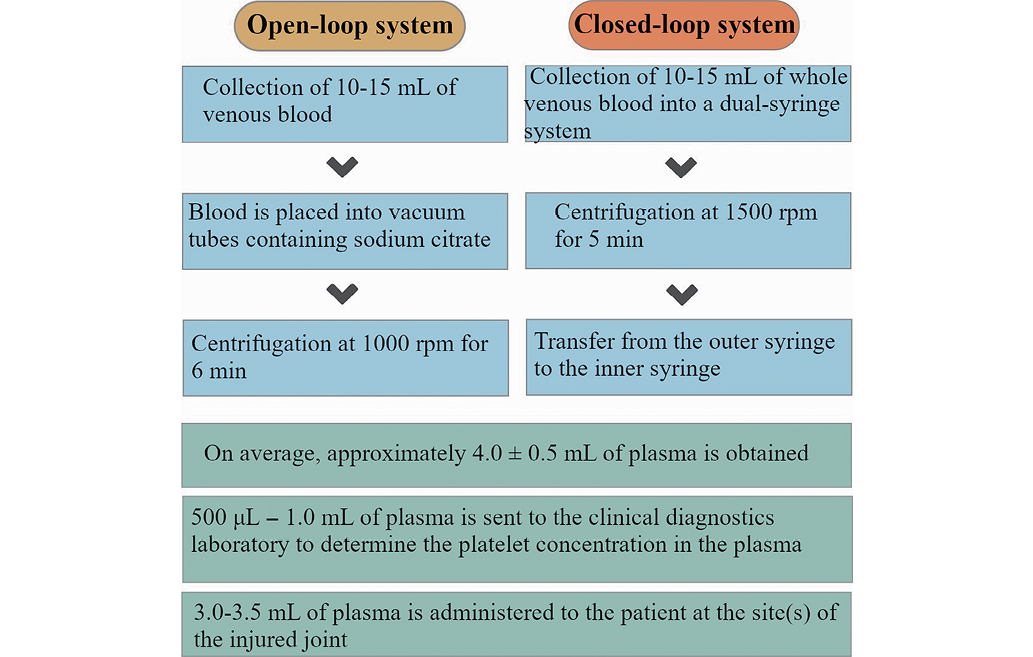
Figure adapted from [8]
Fig. 1. Methods of PRP application for injuries and damage to large joints in underage athletes
Table. Point-of-Care processing methods for platelet-rich plasma
|
Name of Commercial Kit |
Claimed Platelet Increase Fold (Times) |
Platelet Increase Fold (Times) |
Centrifugation Time (min) |
Key Advantages |
Disadvantages |
|
ProofPoint |
No data available |
5.2 |
49 |
More than 4-fold increase in platelet count in plasma |
Transfer via syringe. open system; 2 centrifugation stages |
|
AcCELLerated |
4 |
5.2 |
18 |
More than 4-fold increase in platelet count in plasma |
Absent |
|
Arthrex |
2–3 |
4.2 |
15 |
Reduction of processing time; More than 4-fold increase in platelet count in plasma |
Non-permanent increase in platelet count |
|
Celling |
No data available |
2.7 |
29 |
Usability |
Non-permanent increase in platelet count |
|
Terumo |
3.62 |
4.1 |
24 |
More than 4-fold increase in platelet count in plasma |
Variability of results |
Table prepared by the authors using own data [17]
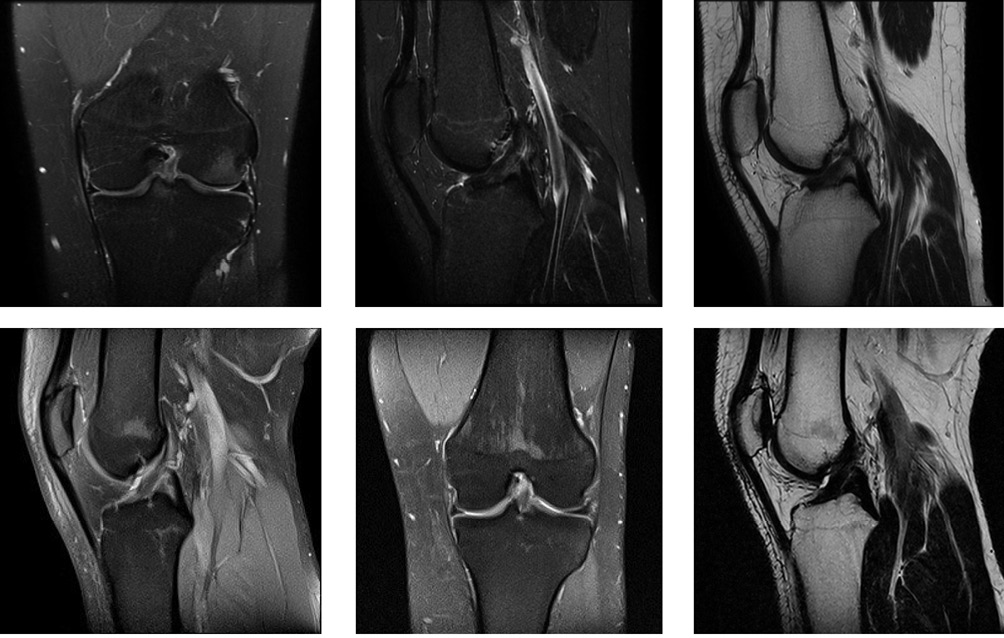
MRI image obtained by the authors.
Fig. 2. Magnetic resonance imaging of the left knee joint: A — after injury; B — after treatment
CLINICAL CASE DISCUSSION
Anterior cruciate ligament (ACL) injury remains a common and severe trauma among professional athletes and sports enthusiasts [2]. Due to the high involvement of the ACL in knee mobility and stability, its injuries are of particular interest to sports medicine specialists, necessitating reduced rehabilitation time, lower probability of long-term complications, and faster recovery and return of athletes to elite sports. In this context, regenerative medicine technologies, including the use of platelet-rich plasma (PRP), hold a special place in orthopedics. Numerous research articles on PRP therapy have been published, demonstrating positive outcomes such as pain relief, stimulation of tissue regeneration, and accelerated healing processes in patients with musculoskeletal injuries [18]. PRP therapy is a minimally invasive method that can be used both as a monotherapy and in combination with conservative treatment. To accurately assess the effectiveness of PRP, comprehensive and dynamic clinical and instrumental examination is required. Thorough history-taking, pain assessment, and physical examination are helpful in determining the most appropriate diagnostic tools. Some studies prioritize magnetic resonance imaging (MRI) for diagnosing ligamentous injuries of the knee joint in children [19].
Indeed, MRI is widely used for evaluating knee injuries, but its accuracy in cases of damage to various structures of the knee joint remains uncertain. However, for ACL injuries, the high sensitivity of this method amounting to 90.4% has been proven [20].
In the presented clinical case, the use of PRP for ACL injury in an underage professional athlete showed favorable results both in terms of pain relief and restoration of functional abilities of the injured limb. It is important to note that this method is safe when procedural requirements are met (asepsis, antisepsis, ultrasound guidance, etc.), cost-effective due to the use of the patient’s own plasma, and yields rapid results. The use of a closed-loop system for PRP preparation minimized potential risks, reduced the consumption of medical supplies, and shortened the time required for transferring PRP between tubes, thereby enhancing economic efficiency.
CONCLUSION
The study presents standardized methodologies for PRP therapy in injuries and damage to large joints in underage athletes. The efficacy of PRP application for ACL injury in a professional beach volleyball athlete was evaluated. A set of trigger points to track dynamic changes during PRP therapy for ACL injuries was theoretically substantiated, including clinical presentation with pain assessment via VAS, physical examination data, results of specific functional tests (Lachman test and anterior drawer test), and MRI diagnostics. The presented clinical case demonstrates the effectiveness of PRP therapy, with positive dynamics on radiological diagnostic results, culminating in complete restoration of the anterior cruciate ligament structure within the period of six months.
Given the existing domestic and international experience of using PRP for diseases and injuries of large joints in older population cohorts, as well as the results obtained in this clinical case, it appears promising to continue the application of PRP in underage athletes with injuries and damage to large joints. Subsequent evaluation of the efficacy of the proposed method should consider injury localization, type of damaged tissue, time since injury, and rehabilitation period, with documentation of clinical and functional dynamics.
1 Decree of the Government of the Russian Federation No. 3081-r dated 24.11.2020 “On the Approval of the Strategy for the Development of Physical Culture and Sports in the Russian Federation for the Period up to 2030”. URL: https://docs.cntd.ru/document/566430492
2 Resolution of the Government of the Russian Federation No. 1661 dated 30.09.2021 “On the Approval of the State Program of the Russian Federation ‘Development of Physical Culture and Sports”. URL: https://base.garant.ru/402891691/
3 List of Instructions of the President of the Russian Federation following the meeting of the Presidential Council for the Development of Physical Culture and Sport dated 29.11.2024, No. Pr-2500. URL: http://www.kremlin.ru/acts/assignments/orders/75738
4 Decree of the President of the Russian Federation No. 145 dated 28.02.2024, “On the Strategy for Scientific and Technological Development of the Russian Federation”. URL: http://www.kremlin.ru/acts/bank/50358
5 Normal Platelet Count in Blood. URL: https://wer.ru/articles/norma-trombotsitov-v-krovi/ (access date: 27.05.2025)
References
1. Rjabov VP, Nurullin IF, Kurmaev ZF, Sungatullin RI, Belov AM Professional injuries and diseases in athletes. Kazan: Kazan Federal University; 2017 (In Russ.).
2. Campbell CJ, Carson JD, Diaconescu ED, Celebrini R, Rizzardo MR, Godbout V, et al. Canadian Academy of Sport and Exercise Medicine position statement: Neuromuscular training programs can decrease anterior cruciate ligament injuries in youth soccer players. Clinical Journal of Sport Medicine. 2014;24:263–7. https://doi.org/10.1097/jsm.0000000000000068
3. Mitchell J, Graham W, Best TM, Collins C, Currie DW, Comstock RD, et al. Epidemiology of meniscal injuries in US high school athletes between 2007 and 2013. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24:715–22. https://doi.org/10.1007/s00167-015-3814-2
4. McFarland EG, Wasik M. Epidemiology of collegiate baseball injuries. Clinical Journal of Sport Medicine. 1998;8(1):10–3. https://doi.org/10.1097/00042752-199801000-00003
5. Fleisig GS, Andrews JR, Cutter GR, Weber A, Loftice J, McMichael C, et al. Risk of serious injury for young baseball pitchers: a 10-year prospective study. The American Journal of Sports Medicine. 2011;39:253–7. https://doi.org/10.1177/0363546510384224
6. Bray CC, Walker CM, Spence DD. Orthobiologics in pediatric sports medicine. Orthopedic Clinics of North America. 2017;48(3):333–42. https://doi.org/10.1016/j.ocl.2017.03.006
7. Godek P. High-volume PRP therapy. Ortopedia Traumatologia Rehabilitacja. 2022;24(1):43–60. https://doi.org/10.5604/01.3001.0015.7806
8. Malanin DA, Tregubov AS, Demeshenko MV, Cherezov LL. PRP-therapy for osteoarthritis of large joints. Volgograd: VolgGMU Publishing House; 2018 (In Russ.).
9. Xiong Y, Gong C, Peng X, Liu X, Su X, Tao X, et al. Efficacy and safety of platelet-rich plasma injections for the treatment of osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Frontiers in Medicine. 2023;10:1204144. https://doi.org/10.3389/fmed.2023.1204144
10. Pontes de Macedo A, Santos Duarte Lana JF, Pedrozo CM, Corrêa Bottene I, De Medeiros JRM, Da Silva LQ. The regenerative medicine potential of PRP in elite athlete injuries. Fortune Journal of Rheumatology. 2020;2:16–26. https://doi.org/10.26502/fjr.26880014
11. Ficek K, Kamiński T, Wach E, Cholewiński J, Cięszczyk P Application of platelet-rich plasma in sports medicine. Journal of Human Kinetics. 2011;30:85–97.
12. Herdea A, Struta A, Derihaci R, Ulici A, Costache A, Furtunescu F, et al. Efficiency of platelet-rich plasma therapy for healing sports injuries in young athletes. Experimental and Therapeutic Medicine. 2022;23(3):1–6. https://doi.org/10.3892/etm.2022.11139
13. Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA Platelet-rich plasma from basic science to clinical applications. The American Journal of Sports Medicine. 2009;37(11):2259–72. https://doi.org/10.1177/036354650934992
14. Medina-Porqueres I, Martin-Garcia P, Sanz-De-Diego S, Gomez-Caceres A, Moya-Torrecilla F, Reyes-Eldblom M, et al. Clinical and functional outcome of meniscal injuries treated with platelet-rich plasma: a single-center case series. International Journal of Environmental Research and Public Health. 2022;19(12):7118. https://doi.org/10.3390/ijerph19127118
15. Zayni R, Thaunat M, Fayard JM, Hager JP, Carrillon Y, Clechet J, et al. Platelet-rich plasma as a treatment for chronic patellar tendinopathy: comparison of a single versus two consecutive injections. Muscles, Ligaments Tendons Journal. 2015;5(2):92–8.
16. Charousset C, Zaoui A, Bellaiche L, Bouyer B. Are multiple platelet-rich plasma injections useful for treatment of chronic patellar tendinopathy in athletes? A prospective study. The American Journal of Sports Medicine. 2014;42(4):906–11. https://doi.org/10.1177/0363546513519964
17. Jildeh TR, Su CA, Vopat ML, Brown JR, Huard J. A review of commercially available point-of-care devices to concentrate platelet-rich plasma. Cureus. 2022;14(8):e28498. https://doi.org/10.7759/cureus.28498
18. Zhang JY, Fabricant PD, Ishmael CR, Wang JC, Petrigliano FA, Jones KJ. Utilization of platelet-rich plasma for musculoskeletal injuries: an analysis of current treatment trends in the United States. Orthopaedic Journal of Sports Medicine. 2016;4(12):2325967116676241. https://doi.org/10.1177/2325967116676241
19. Askenberger M, Arendt EA, Ekström W, Voss U, Finnbogason T, Janarv PM. Medial patellofemoral ligament injuries in children with first-time lateral patellar dislocations: a magnetic resonance imaging and arthroscopic study. The American Journal of Sports Medicine. 2016;44(1):152–8. https://doi.org/10.1177/0363546515611661
20. Li X, Hou Q, Zhan X, Chang L, Ma X, Yuan H. The accuracy of MRI in diagnosing and classifying acute traumatic multiple ligament knee injuries. BMC Musculoskeletal Disorders. 2022;23:43. https://doi.org/10.1186/s12891-021-04976-1
About the Authors
I. V. ZyabkinRussian Federation
Ilya V. Zyabkin - Dr. Sci. (Med.)
Moscow
I. V. Pankratov
Russian Federation
Ivan V. Pankratov
Moscow
A. M. Kovalkova
Russian Federation
Aleksandra M. Kovalkova
Moscow
V. V. Khizhnikova
Russian Federation
Victoria V. Khizhnikova
Moscow
E. V. Zavaleva
Russian Federation
Elena V. Zavaleva - Cand. Sci. (Med.)
Moscow
V. A. Mukhortykh
Russian Federation
Valeriy A. Mukhortykh - Cand. Sci. (Med.)
Moscow
Supplementary files
Review
For citations:
Zyabkin I.V., Pankratov I.V., Kovalkova A.M., Khizhnikova V.V., Zavaleva E.V., Mukhortykh V.A. Injuries and damage to large joints in underage athletes. Therapy with platelet-rich plasma. A clinical case. Extreme Medicine. 2025;27(4):542-549. https://doi.org/10.47183/mes.2025-323

















